New York's highest court of appeals has held that no-fault insurers cannot deny no-fault benefits where they unilaterally determine that a provider has committed misconduct based upon alleged fraudulent conduct. The Court held that this authority belongs solely to state regulators, specifically New York's Board of Regents, which oversees professional licensing and discipline. This follows a similar recent ruling in Florida reported in this publication.
A New Approach to Managing Pain: Thermal Imaging and Infrared Light Therapy
I have been practicing chiropractic in Fairfield, California for over 23 years. Three years ago, I began implementing a new pain management solution in my practice, with the introduction of digital infrared thermal imaging and an infrared light therapy called "photonic stimulation." The imaging technique and complementary treatment modality have assisted me in the diagnosis and treatment of many challenging cases. As a board-certified infrared specialist, I have been able to expand and diversify my existing practice; subsequently, I have experienced an increase in referrals from my patients and other doctors.
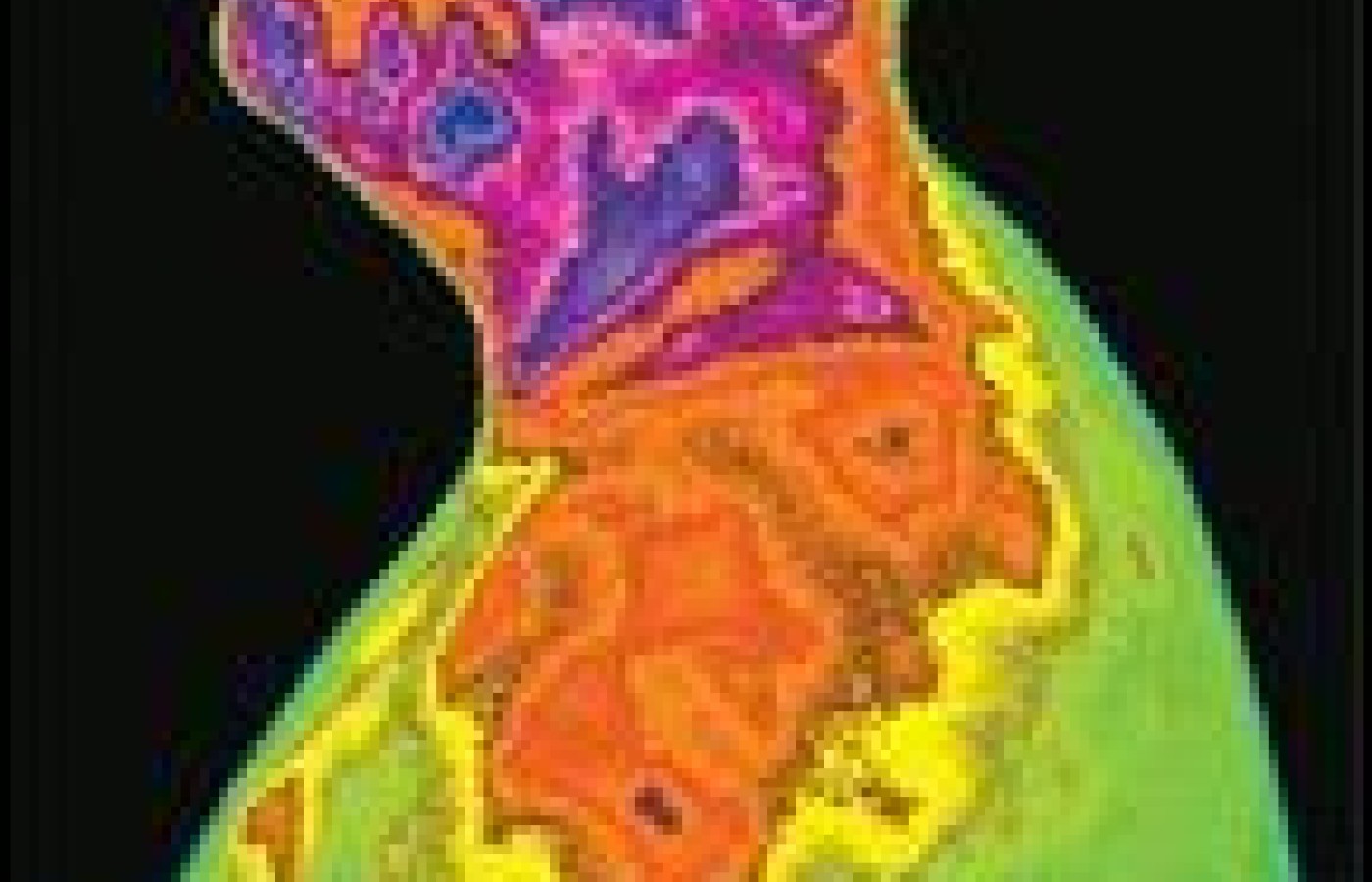
Digital infrared thermal imaging (DITI) is a safe and accurate procedure for measuring and recording surface body temperatures. DITI detects the heat or infrared radiation that is spontaneously emitted from the microcirculation of the skin. These measurements are converted into live images, which, in essence, are a reflection of the autonomic nervous system. Alterations of the neurological and musculoskeletal systems, caused by dysfunction or trauma, can be monitored easily.
The infrared imaging camera assists in performing several professional responsibilities:
- arriving at an accurate diagnosis;
- determining the best type of treatment to administer;
- monitoring the effects and progress of that treatment; and
- evaluating when to terminate treatment.
In the diagnosis of pain syndromes, infrared heat display has the unique ability to image physiology. The chiropractor can "see" the body's physiology and assess the integrity of the peripheral autonomic nervous system. Infrared imaging is the only technique that allows a chiropractor to visualize, with live images, the physiology of the autonomic nervous system. The majority of other diagnostic imaging tests on the market only image anatomy. Chiropractors understand that abnormal function can precede abnormal anatomy; however, we are frequently without a test to measure function.
The infrared imaging modality is used to locate hypo- or hyperthermic areas, establishing an area of physiologic dysfunction. Treatment can then be administered locally using a novel, FDA-approved photonic stimulator, while doing live temporal imaging. Photonic stimulation is now being utilized successfully for the treatment of complex regional (and other) pain syndromes (CRPS), and for soft-tissue injuries.
Many patients come to see me with pain syndromes or soft-tissue maladies, frustrated with ineffective results from other treatments. Some patients simply want confirmation that their pain is real and has a physiological basis. Other patients are seeking alternatives to heavy doses of medication, with hopes that infrared light therapy will provide a drug-free alternative. Thermal imaging and infrared light therapy have enabled me to work with patients who have not been treated effectively with the traditional medical model.
Not only does the thermal imaging camera provide physiological insight into the patient's symptoms, it also allows me to target a treatment for the actual source of the problem, rather than the area where the patient is feeling the pain. The infrared camera further assists me in evaluating the effectiveness of a given treatment protocol by comparing thermal images before and after a treatment. These objective temperature findings are recorded, enabling me to monitor the patient's progress throughout the course of treatment.
The infrared camera I utilize at my clinic detects the infrared heat being emitted from the body, and displays the patterns as a dynamic thermal image on a computer monitor. Because this imaging modality is radiation-free, I have no hesitation in using it as an ongoing assessment tool throughout treatment.
Other imaging modalities I have used in the past, such as X-ray, MRI or CT scans, provide only an anatomical view of the body. These imaging modalities miss the body's physiological signals, which are often the key indicators of neurological dysfunction. It is easy to miss these manifestations of the patient's referred zone of pain, or radicular or direct nerve interference, without a tool to measure the body's physiology. The infrared camera enhances the clinical information obtained in the history, the physical findings, and other tests to establish an accurate diagnosis.
The infrared camera has helped me expand my practice, by enabling me to accurately diagnose and better manage patients with acute and chronic pain syndromes that cannot be discovered through any other means. Many conditions - such as complex regional pain syndromes (CRPS types I and II); sympathetic-maintained pain (SMP); sympathetically independent pain (SIP); soft-tissue injuries; and muscle, ligament and intervertebral disc and joint dysfunction - are clearly discernible with infrared imaging.
I also get tremendous satisfaction from enabling patients to finally see the source of their symptoms on the thermal images, and watching the thermal images change as treatment progresses and their pain abates. This visual representation of healing builds the patient's confidence in their treatment and in the practitioner, which is a powerful patient motivator.
The Thermal Imaging Process
When a patient comes to my office for thermal imaging, I take a series of baseline images, from which I can compare all future thermal images taken throughout treatment. To capture an effective baseline image, I instruct the patients to follow the pre-examination guidelines of the American Chiropractic Association (ACA)
- Avoid hot water exposure while bathing, two hours prior to testing;
- Avoid placing any material of any kind on the skin, such as lotions, bandages, braces or topical analgesics;
- Avoid nicotine and caffeine four hours prior to testing;
- Avoid excessive sun exposure one week prior to testing;
- Coordinate the use or withdrawal of certain medications that have an effect on sympathetic function with the prescribing physician, so they can be withheld 12 -24 hours prior to the evaluation; and
- Avoid all strenuous physical exercise and drinking hot or cold beverages four hours prior to testing.
Once the patient arrives for imaging, he or she is gowned and prepared for study in a thermally controlled room (68°). A minimum of 10 minutes is required to equilibrate the patient to the ambient room temperature. All of these steps are taken to capture the most accurate clinical diagnostic thermal image possible. Fortunately, the new thermal cameras do not require the 20-to-30-minute patient equilibration periods that were necessary 10 to 20 years ago.
The body acts as a thermal reference because of the thermal symmetry of opposite sides. When compared to one another, the sides should be a mirror image within 1ÅC. The thermal emissions are a direct measurement of the blood flow through the microcirculation of the skin. This thermoregulatory skin mechanism is controlled by the sympathetic nervous system. The doctor must be able to recognize this asymmetry.
DITI software now available is quite user-friendly. It is a simple tool for any doctor with a good eye for detail. A doctor can visualize and measure heat differentials with the simple click of a mouse. With the body as its own thermal reference, any temperature asymmetry greater than 1ÅC can be significant. This can easily be spotted and measured with the assistance of the software programs that accompany infrared imaging systems. Again, this thermal data enhances the clinical information obtained from history, physical examinations and other tests, increasing the potential for a more accurate and timely diagnosis. This thermal data also allows for better case management of acute and chronic pain syndromes.
The Thermal or Mechanical Challenge
I typically conduct a thermal or mechanical stress test with patients, after I have observed and stored the initial baseline images on the computer. These tests are effective at producing a reflex response in the sympathetic nervous system, and are intended to elicit a normal, appropriate vasodilatation or vasoconstriction response. This five-minute stress challenge test can involve:
- placing the patient's hands or feet in hot or cold water;
- going through a specific range of motion, such as a lifting or sitting maneuver; or
- another maneuver that elicited a painful response from that patient in the past.
The expected outcome of these specific autonomic stress challenges is to elicit a normal thermal heating or cooling response. An abnormal heating or cooling response is considered suspect.
Infrared imaging with a thermal challenge is one of the most sensitive tests available for evaluating and clinically diagnosing a number of chronic pain syndromes. In fact, thermal imaging, once viewed with a skeptical eye by some medical doctors, is now being adopted by many in the medical community as a state-of-the-art diagnostic tool for confirming complex regional pain syndromes (CRPS types I and II).
The live thermal images serve as a continual reference while treating patients. With each subsequent treatment, one can utilize these images to document and evaluate the patient's physiologic response to treatments. This enables the doctor to quantify the effectiveness of the continued treatments.

Infrared Light Therapy: A New Treatment Modality
Just as the infrared camera has dramatically impacted my ability to recognize pain syndromes, the photonic stimulator has enabled me to treat patients that I couldn't treat effectively before. It emits a highly focused, noncoherent form of infrared light that penetrates the surface of the skin to promote blood flow and circulation; speed healing; improve cell function; and provide pain relief. This application also appears to effectively promote a favorable response with the sympathetic nervous system. The application of light therapy creates a vasoconstriction or a hypothermic response when administered over hyperthermic regions of sympathetic dysfunction. This treatment modality has been shown to be effective at several well-respected clinics throughout the country. Photonic stimulation therapy has a positive effect on treatment outcomes, and can reduce total health care costs in treating painful conditions.
Infrared light therapy has been used worldwide for several decades, but is just beginning to become popular in the United States. A body of research exists on the effects of infrared light from a variety of sources, including NASA.
I have found that photonic stimulation is an excellent alternative to medication, surgery and other treatment modalities. This method of treatment frequently relieves patient pain quickly and effectively, without invasive, costly procedures or side effects.
I use the infrared light modality on a variety of conditions and am frequently astonished by the results that it produces. While it does not have the same dramatic effect on every patient, I have obtained positive results with infrared light therapy treating patients with sports and accident-related injuries, as well as joint; carpal tunnel; TMJ; back; and neck pain.
I have seen the most profound results when treating chronic and severe pain syndromes such as CRPS, for which the patient has often run out of treatment options. After experiencing severe and long-term pain, these patients are ecstatic when their pain is reduced after a few treatments with infrared light therapy. I also have received many referrals, as my patients go on to share their results with other pain sufferers in the community, on the Internet or in support groups.
I use infrared light the same way that I do my adjustments - I try to design the treatment to each patient's condition and complaint. I rely on the infrared images to demonstrate a change that allows me to truly "see" the patient's progress. Whether an affected area is inflamed or suffering from disuse atrophy, the infrared light therapy usually can normalize the sympathetic function to the affected area.
Application of Infrared Light on Trigger Points
In myofascial cases, I focus on specific trigger or tender points by directing the light on the points for 1-5 minutes. These regions are usually hyperthermic and are viewed as a focal "hot" spot on the thermal image. In other cases, I will slowly "paint" the infrared light over the affected area until I begin to see the patient's physiological reaction changing on his or her live thermal images.
A treatment can last from 1-15 minutes, depending on the number of areas I am treating. I will typically treat a patient about three or four times in the first week. If the procedures are successful, based on the patient's improved VAS, physical findings and thermal image improvements, I will continue treatments. Typically, if the infrared light procedure is going to work, the clinician will know within the first two weeks. Some patients respond so well that they are released from further care after this initial set of treatments!
I have found thermal imaging and infrared light therapy to be an important piece of the puzzle in diagnosing and treating patients for whom pain relief is elusive. These devices have helped enhance the loyalty and trust of my patients, which, in turn, have produced referrals of new patients. I also feel that I can offer treatment and care to a whole new group of patients, which enables me to be continually energized and challenged in my chiropractic practice.
Please contact me if you have any questions about thermal imaging or infrared light therapy.
Robert Ensley,DC,CACBII
Fairfield, CA
707-426-3655
robertensley@msn.com