It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
MRA
Since graduating from National College of Chiropractic (now National University of Health Sciences) over 20 years ago (Does this put me in an older generation than many of you?), radiology has changed drastically. In the late 70s and early 80s, computed tomography (CT) was the gold standard for much of musculoskeletal imaging, and magnetic resonance (MR) was just emerging on the scene. Today, MR is essentially the gold standard for much of musculoskeletal radiology, except for a few specific disorders; overall, every imaging modality has progressed by becoming more refined and, of course, more interesting.
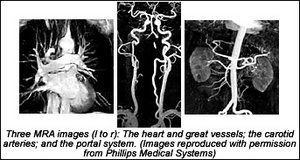
In this and future articles, I will attempt to update myself and whoever is interested on what technology is available, and what is considered state-of-the-art in this millennium. So, let us begin with magnetic resonance angiography (MRA).
Magnetic Resonance Angiography
Conventional angiography remains the gold standard for evaluating the vascular system, but MRA is playing an increasingly important role: providing a safe, cost-effective, and accurate alternative for many angiographic procedures. In many centers, MRA has replaced some diagnostic angiography, and with the recent advances in MR hardware and software, MRA can provide high-quality diagnostic images of arteries and veins throughout the human body.
The use of MR imaging to evaluate vascular structures began soon after clinical MR was introduced in the early 1980s. Blood flowing at normal velocities usually produces little or no signal on spin echo (applying an RF pulse to protons) or fast-spin-echo images, resulting in a natural contrast between flowing blood and vessel walls. This is sometimes referred to as "black-blood imaging" or "black-blood MRA."
Today, MRA is usually used to describe an imaging technique in which blood flow appears bright. The first "bright-blood" technique to achieve widespread clinical use was "time-of-flight" MRA. Early time-of-flight protocols were limited by poor spatial resolution, flow artifacts, and long acquisition times. With the introduction of faster, more powerful gradient systems and improved pulse sequence design, these problems have diminished. Both 2-D and 3-D time-of-flight MRA are now used routinely for many MRA examinations, particularly of the carotid arteries and intracranial vessels.
The introduction of contrast-enhanced (CE) MRA has fueled the rapid growth of MR applications for evaluating extracranial vessels. The problems of signal loss from turbulent flow and in-plane flow saturation have been virtually eliminated with this technique. Three-dimensional CE-MRA techniques can now be performed within a single "breath-hold" on most current imaging systems. This is particularly important for abdominal applications, such as assessment of the renal arteries.
The major disadvantage of MRA is still the spatial resolution. Even with recent advances in MR technology, conventional angiography still provides a higher degree of spatial resolution. However, as MR gradient systems and imaging software continue to advance, this gap will narrow quickly.
Another disadvantage with MRA is that patients with cardiac pacemakers, intracranial vascular clips, and intraocular metallic foreign bodies cannot be imaged safely, because of their strong magnetic fields. Furthermore, patients with severe claustrophobia cannot tolerate placement within the bore of the magnet. The study itself is time-consuming, taking between 1.25 and 1.5 hours to complete. The patient also must be cooperative and still during this time, as movement degrades the images.
The learning curve is also steep, and radiologists need to continue their education. Interpretation of peripheral MRA studies can be a challenge, because of the myriad of potential artifacts and volume of data produced. Over 800 axial images are produced routinely during a single study. These are processed by a computer to produce "3-D projections" that resemble traditional arteriograms. These axial images must be available and reviewed to confirm the findings on "3-D projections."
Artifacts related to surgical clips, movement, pulsatile blood flow, and bowel peristalsis must be recognized to avoid misinterpretation. Not everyone can read these studies; a radiologist who is well-versed in this imaging modality is crucial to gaining a clinically reliable impression.
This is an exciting imaging field, and we are getting close to having the ability to scan a patient without any invasive procedures. The age of "Star Trek" imaging is here. Take a look at what can be done at www.medical.philips.com/main/products/mri/applications/angiography.
Deborah Pate, DC, DACBR
San Diego, California
patedacbr@home.com



