New York's highest court of appeals has held that no-fault insurers cannot deny no-fault benefits where they unilaterally determine that a provider has committed misconduct based upon alleged fraudulent conduct. The Court held that this authority belongs solely to state regulators, specifically New York's Board of Regents, which oversees professional licensing and discipline. This follows a similar recent ruling in Florida reported in this publication.
Gaze Stabilization: Clinical Relevance for DCs
- Failure to properly stabilize our eyes to compensate for rapid head motion can result in blurred vision, nausea, impaired balance, and a greatly increased risk of falling.
- The most common cause of impaired gaze stabilization is advancing age.
- These simple, cost-effective, home-based exercises should be considered by everyone, particularly people who performed poorly during a dynamic visual acuity test.
Although often overlooked, the reflexes required to maintain proper eye alignment during head movements while walking or running involve highly intricate processes. These processes depend on sophisticated interactions among the eyes, cerebellum, brainstem, frontal lobe, vestibular system, and cervical spine.
Keeping our eyes smoothly focused while moving is no simple task because even the simple act of running produces head velocities in excess of 550° per second with head accelerations up to 6,000° per second.1 Failure to properly stabilize our eyes to compensate for rapid head motion could allow our eyes to over- or undershoot specific targets, which can result in blurred vision, nausea, impaired balance, and a greatly increased risk of falling.
The VOR, COR and SEMs
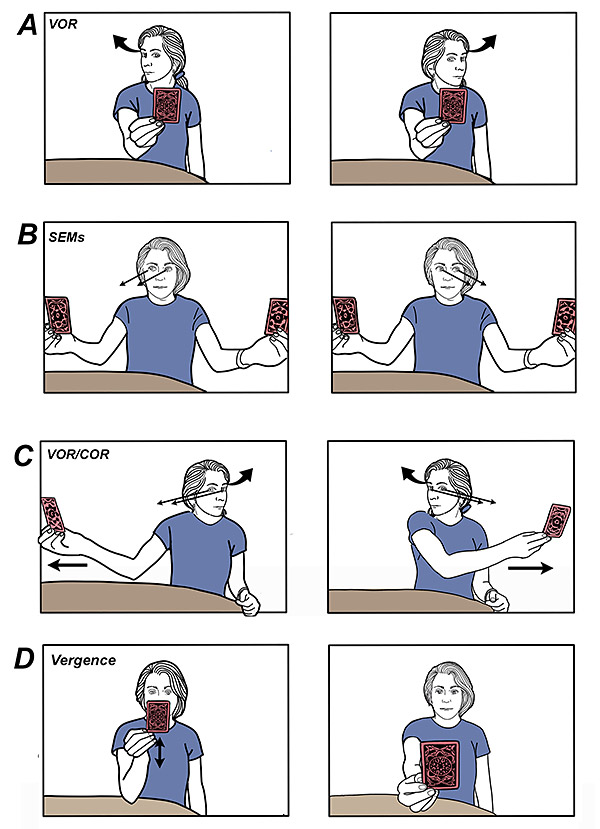
Fortunately, our bodies have three important reflexes that help to stabilize our eye movements to maintain crisp and clear vision no matter how fast we are moving: the vestibulo-ocular reflex (VOR), cervico-ocular reflex (COR) and saccadic eye movements (SEMs).
As the name implies, the VOR receives information regarding head accelerations from our vestibular system that activate eye muscles to move in the opposite direction of head movement: e.g., when you turn your head to the right, both eyes will automatically turn to the left to maintain a stable image on your retina. (Fig. 1, VOR)
While the VOR transmits data regarding head motion, the COR transmits proprioceptive information regarding accelerations of the torso and neck to the cerebellum and vestibular nuclei, which activate the eye muscles to counteract the perceived head and neck rotation. (Fig. 1, COR)
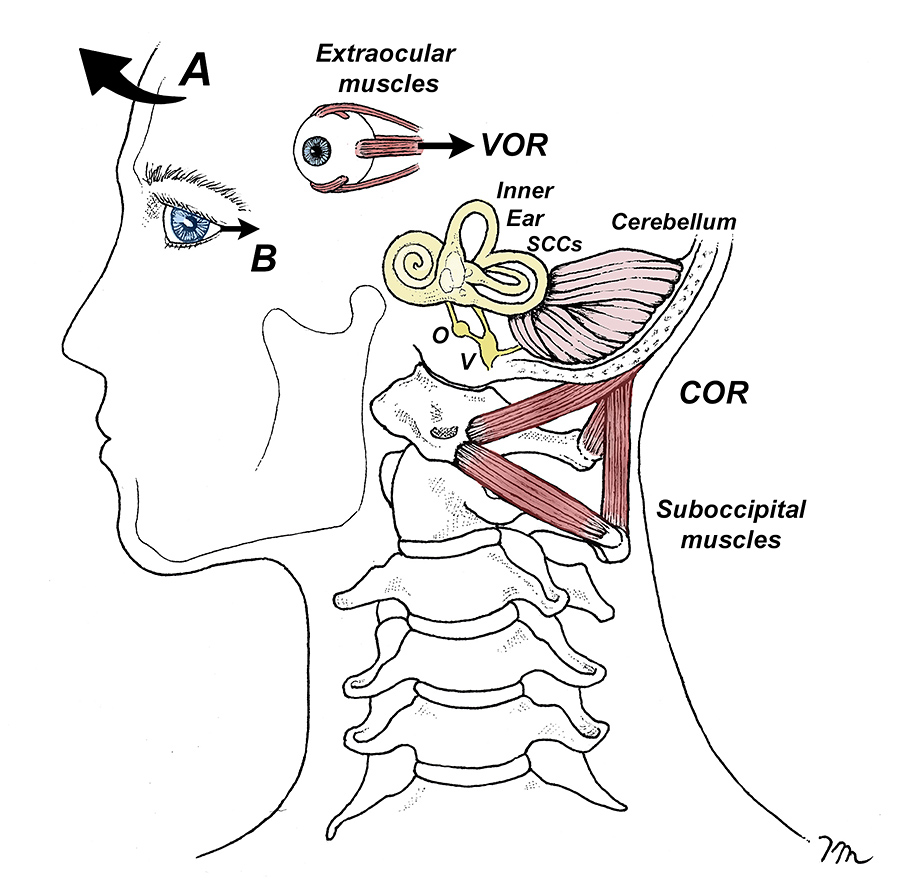
The suboccipital muscles in the upper neck play a key role in the COR because of their high concentration of muscle spindles, which provide detailed position-sense information regarding head movements and accelerations. The density of spindles in these muscles is surprising: while most muscles possess an average of 2-4 spindles per gram of muscle, the suboccipital muscles possess nearly 10 times that amount, averaging between 30 and 40 spindles per gram.2
The high spindle density allows the suboccipital muscles to provide the COR with extremely detailed information regarding all aspects of head position and motion.
The final factor necessary for smooth gaze stabilization is properly functioning saccadic eye movements. Because SEMs are controlled by the frontal and medial eye fields and superior colliculus of the midbrain, and these nerve pathways have direct access to the oculomotor sections of the brainstem, SEMs are capable of producing lightning-fast changes in eye position that allow us to immediately switch our gaze from one target to another.3
Given the sheer volume of information present in our visual fields while walking and running, it’s not surprising that the typical person has more than 170,000 saccadic eye movements per day and about 5 billion in an average lifetime.3
Gaze Stabilization and Age
Despite the complexity of the gaze stabilization system, it tends to function pretty smoothly, especially when we’re young. While the system can malfunction as a result of vestibular disorders, head trauma, a variety of neurodegenerative conditions, and even chronic neck pain,4 the most common cause for impaired gaze stabilization is advancing age.5-6
Researchers from Russia note that as we age, there is a decrease in the number of neurons in the basal ganglia, cerebellum and spinal cord that can negatively affect gaze stabilization by delaying the speed of SEMs.5
The age-related deterioration of gaze stabilization was proven in 2022 when the Korean researcher Youngsook Bae evaluated 128 individuals between the ages of 65 and 89, measuring their SEM speed with a high-speed eye-tracking device, and evaluating balance by performing the functional reach test, the timed up-and-go test, and measuring walking speed.6 After detailed analysis, the author conclusively demonstrated that as age increased, SEM speed significantly decreased, and that reduced SEM speed was strongly correlated with impaired balance and reduced walking speed.
Bae emphasizes that this was the first study ever to show correlation between SEM and balance, and specifically states that the reduced SEM speed results in an “inadequate response to rapid external environmental stimuli and may be a factor that deteriorates the ability to balance in older adults.”
Although Bae used expensive high-tech eye-tracking technology to analyze SEMs, it is also possible to accurately evaluate the overall health of the SEMs with a dynamic acuity test. To perform this test, download a Snellen eye chart and place it 10 feet away. Set a metronome to 120 bpm and rotate your head 20°-30° with each beat. Record the last line you can read before the letters blur.
Repeat with your head still and compare results. A difference of more than three lines suggests vestibulo-ocular reflex impairment – which means gaze stabilization exercises may help.
Gaze Stabilization Exercises: Clinical Relevance for DCs
More than 15 years ago, Morimoto, et al.7 had healthy young adults perform the gaze stabilization exercises illustrated in Figure 2 and noted that these simple exercises not only improved dynamic visual acuity, but also postural stability while standing with active head rotation. Additional research has shown that simple eye movement exercises can improve balance ability and confidence8 and even improve cognitive function in healthy older adults.9
Roh and Lee10 recently demonstrated that even older individuals with mild cognitive impairment benefit from eye exercises, as in addition to improved cognition, eye exercises improved balance and affected the overall quality of life in older adults with and without cognitive impairment.
Enhancing balance in older adults with cognitive impairment is particularly important, as research indicates these individuals are five times more likely to experience falls compared to cognitively healthy older adults.11
Last, but not least, because research consistently finds that adding gaze stabilization exercises to conventional balance rehabilitation results in significantly reduced fall rates,12 these simple, cost-effective, home-based exercises should be considered by everyone, particularly people who performed poorly during the dynamic visual acuity test.
When you consider that nearly 900,000 Americans are hospitalized annually as the result of a fall, it seems that performing a few simple eye exercises just a few times per week is a small price to pay to improve balance, walking speed and mental acuity as we age.
References
- Schubert MC. Compensatory Strategies for Vestibulo-Ocular Hypofunction. In: Vestibular Rehabilitation, 3rd Edition. Philadelphia, PA: FA Davis Co. 2000:265-71.
- Kokkorogiannis T. Somatic and intramuscular distribution of muscle spindles and their relation to muscular angiotypes. J Theoretical Biol, 2004 Jul 21;229(2):263-80.
- Schiller PH, Tehovnik EJ. Neural mechanisms underlying target selection with saccadic eye movements. Prog Brain Res, 2005 Jan 1;149:157-71.
- Johnston J, Daye P, Thomson G. Inaccurate saccades and enhanced vestibulo-ocular reflex suppression during combined eye–head movements in patients with chronic neck pain: possible implications for cervical vertigo. Front Neurol, 2017 Jan 30;8:23.
- Litvinova A, Ratmanova P, Evina E, et al. Age-related changes in saccadic eye movements in healthy subjects and patients with Parkinson’s disease. Human Physiol, 2011 Mar;37(2):161-7.
- Bae Y. Decreased saccadic eye movement speed correlates with dynamic balance in older adults. Int J Environ Res Public Health, 2022 Jun 26;19(13):7842.
- Morimoto H, Asai Y, Johnson E, et al. Effect of oculo-motor and gaze stability exercises on postural stability and dynamic visual acuity in healthy young adults. Gait Posture, 2011 Apr 1;33(4):600-3.
- Park J. The effects of eyeball exercise on balance ability and falls efficacy of the elderly who have experienced a fall: a single-blind, randomized controlled trial. Arch Gerontol Geriatr, 2017;68:181-185.
- Parker A, Relph S, Dagnall N. Effects of bilateral eye movements on the retrieval of item, associative, and contextual information. Neuropsychol, 2008 Jan;22(1):136.
- Roh M, Lee E. Effects of gaze stability exercises on cognitive function, dynamic postural ability, balance confidence, and subjective health status in old people with mild cognitive impairment. J Exer Rehab, 2019 Apr 26;15(2):270.
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med, 1988;319:1701-1707.
- Hall CD, Heusel-Gillig L, Tusa RJ, Herdman SJ. Efficacy of gaze stability exercises in older adults with dizziness. J Neuro Phys Ther, 2010 Jun 1;34(2):64-9.


