It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Achilles Tendon Rupture: The Chiropractor's Role
- Presently there is no consensus on the best treatment for Achilles tendon rupture; and its management is still controversial.
- An acute rupture of a healthy tendon can be successfully treated either conservatively or operatively.
- The rehabilitation component is an opportunity where chiropractors can play a key role.
The Achilles tendon, which is about 12–15 cm long, is comprised of both the gastrocnemius and the soleus tendons. It arises at the middle of the calf and rotates approximately 90 degrees laterally during its course to insert on the posterior aspect of the calcaneal tuberosity. It is reported to be the strongest tendon in the body, but also the most frequently injured.
Presently there is no consensus on the best treatment for Achilles tendon rupture; and its management is still controversial. The treatment options are conservative treatment and surgical repair. With either treatment, be it conservative or surgical, Achilles tendon tears necessitate prolonged recovery and rehabilitative management. Even with the best treatment, the patient is generally left with a 10% to 30% reduction in functional calf strength and endurance.1
The Calgary Guide to Understanding Disease is an excellent tool for reviewing the causes and clinical presentations associated with this diagnosis. [View Here] The assessment missing that I might have included is the imaging aspect for the diagnosis of this entity. And I certainly would like to see a diagram demonstrating treatment protocol as to when surgical intervention is necessary. But unfortunately, there is no consensus.
Assessing Tears: Imaging
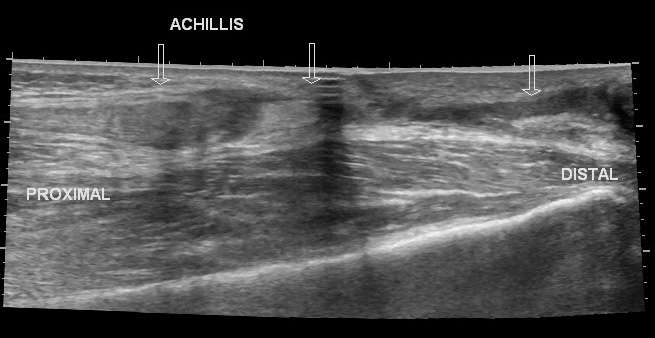
Tendinopathy and full-thickness tears may be assessed effectively both on MRI and ultrasound. MRI is superior to ultrasound in detection of partial tears and for postoperative assessment. There are other pathological processes that can be assessed with MRI, but they are not discussed here. (For a more in-depth discussion of MRI assessment, see reference #2.)

The Achilles tendon is covered by the paratenon. It is not visible on MRI, but this structure can be seen on ultrasound by an experienced sonographer. The paratenon is highly vascularized; thus, it is important in the healing of a torn Achilles tendon. (For a more in-depth understanding of ultrasound of tendons and the anatomy, see reference #3.)
Ultrasonography is the most used imaging modality for the assessment of injured or painful Achilles tendon. Ultrasound is easily accessible and an inexpensive modality; however, it is operator dependent, whereas MRI depends on an optimal protocol that can be followed by any MRI technologist.
The indications for MRI and US in the assessment of the Achilles tendon overlap. US is as good as MRI in detection of tendinopathy and full-thickness tears. (See images) Postoperative complications, such as calcaneus fracture, infection and abscess formation, tendon, or graft rupture, are better assessed via MRI.
See link below comparing the use of MRI vs Ultrasound:
www.ncbi.nlm.nih.gov/pmc/articles/PMC8039565/table/tbl0005/?report=objectonly
(To see all the images from this study, click here.)
It is my conclusion that if the patient is young and there are no other health issues, except for a traumatic injury, an ultrasound is the modality of choice. However, if the patient is older, has other health issues, and the history of injury is not necessarily due to a traumatic incident, MRI is the obvious modality of choice. Of course, not every case is as clear cut, so in general, I would tend to choose the MRI study, because I am more comfortable looking at the anatomy with this modality.
Causation, Presentation
Rupture of the Achilles tendon is a common sports injury. Typically, patients are male, over the age of 40 years and have recently returned to social sports that involve quick running and stopping. The patient usually hears a sudden "snap" in the calf or believes that they were hit from behind.
Achilles tendon rupture may occur in any section of the tendon. The most common site of a rupture is at the midportion of the tendon at 5-6 cm from the insertion. Most patients experience pain in their calf and inability to plantarflex.
There are two main theories concerning rupture of the Achilles tendon: 1) It is due to degeneration of the tendon. 2) Unusual stresses applied to an unconditioned tendon cause a rupture. Partial ruptures of the Achilles tendon may occur in any part of the tendon and may be located at the surface or intratendinous. Most partial surface tears may be related to tendon degeneration.
Treatment, Rehabilitation and the Role of the Chiropractor
Once diagnosis of ruptured Achilles tendon is made with imaging and clinical findings, the real problem is, what are the treatment options? In general, when the tear is due to acute trauma, the older the patient is, the more likely they will receive conservative treatment, in order to avoid complication from surgical intervention. However, since there is no consensus about initial treatment and management, it is ultimately up to the clinician and the patient.
Acute Achilles tendon ruptures should be differentiated from ruptures that occur as the result of chronic degeneration of the tendon. An acute rupture of a healthy tendon can be successfully treated either conservatively or operatively.4
Irrespective of the treatment method, however, rehabilitation is a crucial component of treatment. The rehabilitation component is an opportunity where chiropractors can play a key role. As with many disorders, managing patient health care is a team effort.
The specifics of the rehabilitation protocol may vary. The focus of rehabilitation is on preventing re-rupture for the first two months after injury and improving calf muscle strength for the next month. For the following three months (between 3-6 months after injury), rehabilitation efforts are directed toward a return to activities of daily living (including sports) through vigorous strengthening and proprioceptive exercises.
Two Cases (One Surgical, One Conservative)
Presently I am following the progress of two patients who ruptured their Achilles tendon within a few months of each other due to acute trauma. One is a 63-year-old male who ruptured his tendon during a martial-art sparring incident. He is very athletic, was a gymnast in his youth, and is now a fitness instructor and continues to train for various sporting events.
He chose the surgical treatment. Unfortunately, due to insurance problems the surgery was performed three weeks post-injury; prior to the surgery he was in a weight-bearing boot. After surgery, he again wore the boot for two weeks with no weight-bearing; rehab treatment was next and continues.
He is presently nine months post-op and continues with aggressive rehab. The prognosis is excellent, but assessment at one-year post-op will determine the extent of his recovery.
The second patient is an 80-year-old male who ruptured his tendon playing tennis. This patient is an avid tennis player, still playing singles at 80. He opted for the conservative treatment. He received similar rehabilitation as the first patient with the initial few weeks in a boot with no weight-bearing, followed by functional rehabilitation. Seven months post-injury, he is back to playing an easy game of tennis. (What constitutes an easy game, I’m not certain).
Neither patient is at 1-year post-injury, so I can’t report on the extent of their recovery. What is interesting is that both had a complete rupture at the mid-portion of the tendon confirmed on MRI. Both appear to have had a good result and the prognosis is good, if not excellent, for both. Both certainly were fit and had healthy tendons to start with.
One had a chiropractor managing their rehab and the other a physical therapist. Neither patient had pain with the initial injury; they only experienced the “pop” and both knew immediately that they had ruptured the tendon. Even though the primary treatment was different, both received similar rehabilitation.
Take-Home Points
Acute Achilles tendon ruptures should be differentiated from ruptures that occur as the result of chronic degeneration of the tendon. An acute rupture of a healthy tendon can be successfully treated either conservatively or operatively. Irrespective of the treatment method, however, rehabilitation is a crucial component of treatment.
Therefore, a patient’s adherence to rehabilitation should be taken into consideration in determining a treatment strategy. Rehabilitation during the first six months after injury is of great importance, regardless of initial treatment. Chiropractors should be referred to more often for the rehabilitation of Achilles tendon tears; especially those with advanced training in sports and rehabilitation.
References
- Dams OC, van den Akker-Scheek I, Diercks RL, et al. The recovery after Achilles tendon rupture: a protocol for a multicenter prospective cohort study. BMC Musculoskelet Disord, 2019 Feb 11;20(1):69.
- Szaro P, Nilsson-Helander K, Carmont M. MRI of the Achilles tendon - a comprehensive pictorial review. Part one. Eur J Radiol Open, 2021 Mar 26;8:100342. Read Here
- Mascarenhas S. A narrative review of the classification and use of diagnostic ultrasound for conditions of the Achilles tendon. Diagnostics, 2020 Nov 13;10(11):944. Read Here
- Park SH, Lee HS, Young KW, Seo SG. Treatment of Acute Achilles Tendon Rupture. Clin Orthop Surg. 2020 Mar;12(1):1-8. doi: 10.4055/cios.2020.12.1.1. Epub 2020 Feb 13. PMID: 32117532; PMCID: PMC7031433.



