It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Somatosensory Evoked Potentials in Chiropractic Clinical Practice -- Part I
Evoked potentials are a type of objective and noninvasive electrodiagnostic testing that are used by both medical and chiropractic doctors. There are three basic types of evoked potential studies: visual evoked potentials (VEPs), brainstem auditory evoked potentials (BAEP), and somatosensory evoked potentials (SSEP), which also includes dermatomal somatosensory evoked potentials (DSSEP). SSEP and DSSEP are most applicable to chiropractic practice and will be the central focus of this three part series on evoked potentials (EPs). Part I will include a general introduction to evoked potentials, Part II will focus on cervical/upper extremity SSEP and DSSEPs, and Part III will discuss lumbar/lower extremity SSEP and DSSEPs. SSEPs, DSSEPs, VEPs, and BAEPs are all tests that measure their respective sensory systems.
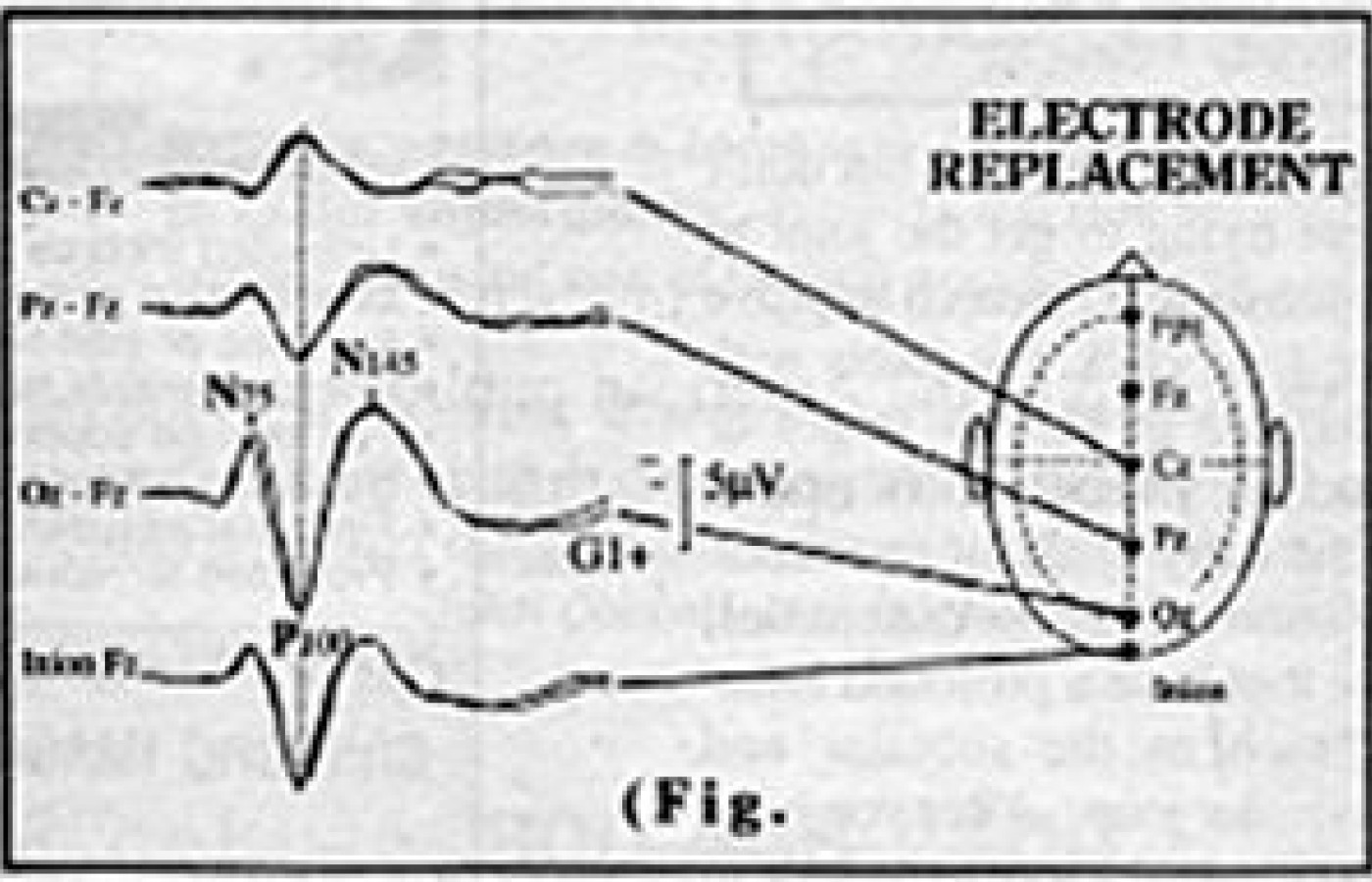
VEPs measure the integrity, of the visual sensory conduction system by stimulating the patients eyes and visual cortex with a flashing checkerboard screen that changes its patterns (pattern reversal shift). A positive peak occurring at 100 milliseconds after stimulation (P100), is the most common waveform analyzed in VEP studies for absolute latency, amplitude, and interocular latency, and amplitudes.
An upper limit of 8-10 milliseconds from right to left is within normal limits. The most common changes in P100 are seen in MS with latency delays > 10 msec.
BAEPs examine the integrity of the auditory sensory conduction pathways by placing headphones on the patient and stimulating the patient with a series of audible clicks. Electrodes then record the cortical activity. Five waveforms are analyzed for their latency, and these are labeled Wave 1 through Wave 5.
BAEPs are sensitive and helpful in the diagnosis of MS, acoustic neuromas, and cerebellar pontine angle tumors.
SEPs measure peripheral sensory nerve function, nerve root function, dermatomal integrity, central conduction pathways, and thalamocortical function. A peripheral mixed or sensory nerve, or dermatomal region is stimulated many times and then averaged to eliminate electrical noise. Electrical waveforms are measured and picked up at different proximal locations with special surface electrodes and are recorded for absolute peak latency, amplitude, and interpeak latencies. Peak latency is the time measured from stimulus onset to the point of maximum amplitude of a negative or positive peak. Amplitude is the vertical distance representing voltage difference between a peak and the horizontal. SEPs have been shown to be an accurate method of assessing axonal continuity. SEPs are very sensitive to help localize lesions in the peripheral and central segments of the sensory pathways. SEPs consist of a series of recorded upward or downward deflections called peaks or waves, that can be analyzed for waveshape, amplitude, latency, and distribution. They are usually labeled for polarity (negative or positive) and the normal time frame at which they occur (i.e., N9; the first negative or upward deflection in an upper extremity mixed nerve SEP occurring at 9 milliseconds at Erbs point). Some only label peaks by polarity and the sequence in which it occurs (i.e., N1, P1).
SEP findings that are considered abnormal include:
- Absent waves or peaks
- Delayed absolute latencies
- Increased interpeak latencies
- Latency delays from right to left
The patient is his own control, and latencies/interpeak latencies are compared from right to left and should fall within 2-3 standard deviations of published normal values. Absolute latencies can be referenced to published normals as well, however in the lower extremity studies patient height must be accounted for. SSEPs and DSSEPs can be helpful in the diagnosis of peripheral nerve entrapments, radiculopathy, plexopathy, thoracic outlet syndromes, and other neurological disorders (i.e., multiple sclerosis).
David BenEliyahu, DC, CCSP, DABCT
Selden, New York
Editor's note: Part II (upper extremity SSEPs and DSSEPs) will be presented in the 7-29 issue. Part III (lower extremity studies) will appear in the 9-1 issue.