It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Best Practice: Disc Herniations With Serious Neurological Deficits
- The benefits outweight the harms for conservative care in patients with severe sciatica who would qualify for surgery in most hospitals.
- Spinal surgeons may assert that keeping patients with two or more nerve root compression signs away from surgery is unsafe. However, according to research, it appears to be a safe strategy.
- Research also suggests chiropractic spinal manipulation can deliver a large, clinically important pain reduction with no adverse events in patients with sciatica with disc protrusion.
A patient tells you that a neurosurgeon has told her she has severe sciatica that requires immediate surgery, because she has nerve damage that could progress and become permanent, and even could lead to permanent foot drop. This patient has leg pain of 6/10 with motor and sensory deficits. She has had these symptoms for three months. The neurosurgeon has recommended surgery this week.
The patient wants to know if her condition will become permanent or lead to worse symptoms. Should she proceed with the immediate surgical approach? How do you respond? What does the current research demonstrate? Let’s investigate the benefits and harms of conservative care in patients with severe sciatica who would qualify for surgery in most hospitals.
This was a single-blind, randomized, clinical, controlled trial that compared eight weeks of spinal rehab (therapeutic spinal stabilization exercise) versus sham exercise (low-dose exercise unrelated to the back).1 This study was published in Spine. The research team consisted of one medical doctor and one PhD researcher.
One hundred and eighty-one patients with radicular pain below the knee were examined at baseline with the following findings:
- Positive SLR at 30 degrees: 94.4%
- Motor deficits in leg: 51.3%
- Disturbed sensibility in leg: 80.8%
- Asymmetric reflexes in leg: 54.7%
The patients in this study would be considered surgical candidates in most hospitals, because 95% of them had at least two positive nerve root compression signs (65% had three or four positive nerve root compression signs). The graph demonstrates the results of this study at one year based on Patient Global Assessment.
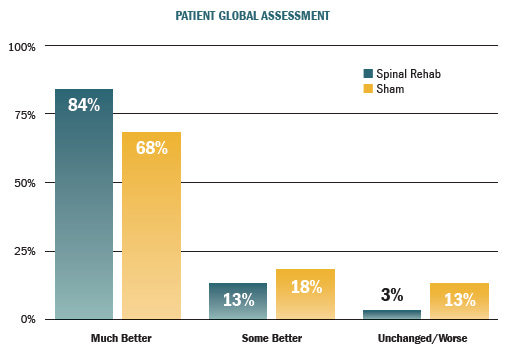
These patients had symptoms and clinical findings that would qualify them for surgery in most hospitals, and yet they experienced highly important clinical improvements in all outcome measures immediately after treatment and at one year after treatment.
Both groups demonstrated improvement in six outcome measures. The active treatment group demonstrated better scores than the control group in four of the six outcome measures. At the one-year follow-up, 91% of patients reported being better or much better. These results were better than those reported for surgical interventions. Only 3% of the patients had increasing symptoms and were referred to surgeons.
Spinal surgeons may assert that keeping patients with two or more nerve root compression signs away from surgery is unsafe. However, according to this clinical trial, it appears to be a safe strategy. No patients developed cauda equina syndrome or severe paresis; and the rescue medication, when needed, was only mild analgesics such as acetaminophen or NSAIDs.
Patients who had suffered for a longer period of time with neurological symptoms experienced results similar to those who had not suffered as long. Results for patients who had sciatica for 3-6 months were just as favorable as results for those who had sciatica for 1-3 months.
A common rationale by spinal surgeons for performing surgery for patients with herniated discs is the belief that surgery brings faster pain relief and return to normal activities. That rationale is not supported by the results of this clinical trial, because after eight weeks of treatment, 74% of the therapeutic spinal stabilization exercise group and 60% of the sham exercise group were back at work (and many had been working throughout the treatment period).
Other research supports these findings. McMorland, et al., found that delaying surgery in patients with severe sciatica secondary to lumbar disc herniation does not adversely affect patient outcomes.2 And Santilli and his medical team demonstrated that chiropractic spinal manipulation can deliver a large, clinically important pain reduction with no adverse events in patients with sciatica with disc protrusion.3
These research studies present compelling data that it is reasonable and safe to encourage patients with radiculopathy due to a lumbar disc herniation to continue nonoperative treatment, unless they develop severe neurologic signs or have intolerable symptoms. Most people with significant neurological symptoms secondary to disc herniations will not need surgery.
References
- Albert HB, Manniche C. The efficacy of systematic active conservative treatment for patients with severe sciatica: a single-blind, randomized, clinical, controlled trial. Spine, 2012;37:531-42.
- McMorland G, Suter E, Casha S, et al. Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. J Manipulative Physiol Ther, 2010;33:576-84.
- Santilli V, Beghi E, Finucci S. Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion: a randomized double-blind clinical trial of active and simulated spinal manipulations. Spine J, 2006;6:131-7.