It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Help Athletes Before the Pain
I have been a student of sports injuries for 41 years. I've been injured and I've helped the injured. I've become intimately aware of the many ramifications that are byproducts of being injured. Most never want to think about injuries until they're injured. Then the topic rises immediately to the top of the list.
I've been fortunate over the years to witness some athletes understand my message and take action. I encourage all athletes to receive a thorough biomechanical exam immediately, and don't equate getting examined with being injured. I've had many parents bring their 12-year-old sons or daughters to our office for an examination despite the fact the young athlete has never been injured.
Case Study: 13-Year-Old Female Basketball Player
This young girl came to my office for an examination even though she's never really suffered any injuries. She plays basketball, soccer and softball, and was a triplet born prematurely. Her father told me she was the third born and never turned in the womb, producing a severe reactive torticollis at birth that took a great deal of physical therapy to normalize. There are no signs of it today.
In looking at an athlete biomechanically, we must remember the human structure is an architectural structure influenced by gravity, aging and stress. There are many findings that can be detected even in the absence of symptoms.
The Biomechanical Exam
I begin this exam with the patient standing, shoes off. I insert three fingers underneath each medial arch to detect if the arches have fallen or are higher than normal, and if right and left appear to be the same height or are different. I then look at the Q angle of the knees, especially in young female athletes.
This young athlete had greater collapse of her left medial arch and a slightly increased Q angle of the left knee. Those two findings are often associated with each other.
I performed a series of range-of-motion tests, as well as standardized orthopedic tests. There was much restriction bilaterally on the Patrick-Fabere test, worse on the left. With the patient in the supine position, the toe-in test was greater on the left.
While testing cervical and lumbosacral range of motion, I asked this young athlete if she ever gets headaches. Knowing she had a severe torticollis at birth, there may be some residual cervical spine issues that have never been addressed. Her father answered for her: "I always have a bottle of Aleve in the car because she has headaches four or five times a week."
Scanning and Imaging
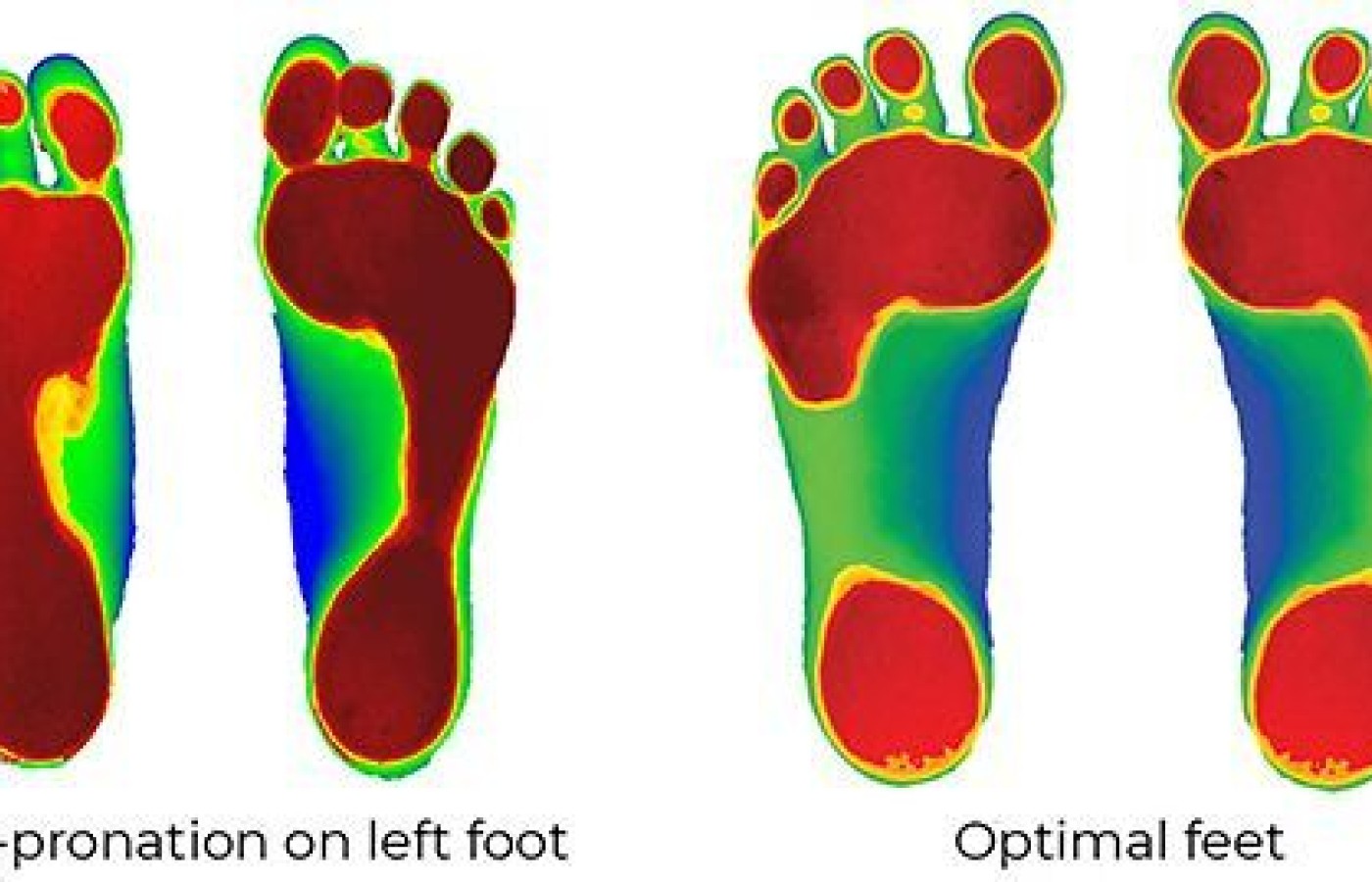
The key to success in both knowing the details of a patient's biomechanics and communicating this information to a patient is, you must have visual evidence. That's what digital scanning of the feet and biomechanical X-rays of the structure provide. Without this information, you can't know the detailed biomechanics that will affect this young athlete's life.
Upon scanning the feet, I first saw that the patient's feet have collapsed relative to optimal feet. (Fig. 1) Second, I saw the left foot has collapsed more than the right foot. There is increased weight-bearing through the left side of the body as compared to the right side of the body, causing the left foot to collapse more over time.

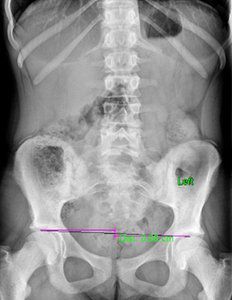
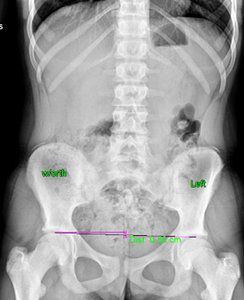
I then looked at her X-rays. The most important view is the A-P L-S. We took the first series barefoot. On this view, I first looked at femoral head height. She had a 6.8 mm femoral head height difference, higher on the right. (Fig. 2) On her lateral L-S view, she had a lumbarization, removing the ability to know exactly what her Ferguson's center of gravity showed, as well as her sacral base angle. On lateral cervical (Fig. 3), she had a straight cervical spine, often associated with chronic headaches. The open-mouth view (Fig. 4) showed the significant imbalance between atlas and axis.

Based on the digital laser foot scan, I ordered full-length stabilizing orthotics with three-arch support. Once the orthotics arrived, I put them in the patient's shoes and re-took the A-P L-S view to see how the orthotics affected femoral head height. The repeat X-ray of the A-P L-S showed there is now a 5.0 mm femoral head height difference, (Fig. 5), showing orthotics help reduce the difference. However, a heel lift was still needed. I applied a 5 mm heel lift to the left orthotic.
General Recommendations
Middle- and high-school athletes are always under tremendous musculoskeletal and neurological stress. The alignment of the teeth can't be more important than the alignment of the neuromusculoskeletal system, but society has not been educated to this fact. We need to make an evaluation like this mandatory for all middle- and high-school athletes, and address biomechanical faults, not just symptoms. The goals I have with my young patients are to "fix" the feet with custom orthotics, then level the hips, and if a lift is needed, provide it.
I then want to recommend spinal / pelvic care, which consists of chiropractic adjustments. Our goal is to ensure mobilization of all joints of the body, as well as affect the relationship between atlas and axis. Increasing the cervical curvature is also a goal.
It is my opinion that this young girl's headaches are directly due to the imbalanced relationship between atlas and axis, and that this imbalance originates in the feet and leg length. To gain maximum benefits of upper cervical adjusting, the feet and leg length must be addressed.
Food for Thought
All middle- and high-school student-athletes get a medical exam prior to their sport season, looking at eyes, ears, nose and throat. Virtually no musculoskeletal or biomechanical tests are performed. The primary reason: Very few professionals are qualified to evaluate or treat biomechanics. Chiropractic is the most educated and qualified profession, and should begin a mass education program to alert this age group that much more can be done proactively, not just reactively.
A biomechanical exam would identify many future injuries and corrective changes could be made sooner, rather than later. This approach would drastically reduce injuries and the costs associated with these injuries, not to mention the massive benefits it would bring to the chiropractic profession.