It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Why Take X-Rays When You Already Have an MRI?
Let's clear up the issue regarding the efficacy of plain-film studies when an MRI study has already been performed. I review imaging studies primarily for chiropractors, and often their patients have been to other health care providers before finding their way to a DC. Many patients believe an MRI is a better diagnostic study than plain-film X-rays, which is not always the case.
The Benefits of X-Ray for Musculoskeletal Disorders
If the patient has a musculoskeletal disorder, often the X-ray study is the best imaging tool for assessing the biomechanical problems. Plain films can be performed as a kinetic study, i.e., in flexion and extension. The X-ray allows for biomechanical assessment of the bony structures and how they interrelate and articulate. Radiographs also can be performed in a weight-bearing position, therefore allowing for the assessment the joint space under the influence of gravity.
Yes, X-rays primarily demonstrate the osseous structure, whereas an MRI demonstrates soft-tissue anatomy (tendons, muscles, ligaments, cartilage, etc.). However, most MRI studies are performed in a non-weight-bearing position and bony structures are not clearly delineated. And let's not forget that X-rays of one region cost less than $100, whereas an MRI can cost more than $500.
The other issue that is often ignored is that too much imaging isn't a good idea! Cost aside, inappropriate imaging can expose patients to the inconvenience and harm created from the cascade of diagnostic and therapeutic interventions that often follow identification of a lesion that turns out to be only an incidental finding and of no clinical significance.
- X-rays produce high-resolution, two-dimensional images and provide a quick, low-cost means of assessing bone and joint disease and soft-tissue calcification.
- Radiography is still the first imaging tool used to assess suspected bone pathology, before other imaging modalities such as MRI or CT.
The Danger of the "Normal" MRI

I often review films after a patient has been in a car accident and is experiencing persistent neck pain and other symptoms. An MRI was ordered and shows nothing of significance; in fact, the report reads that there is no evidence of trauma or pathology: normal study. If the case ultimately goes to litigation, as can sometimes occur, it becomes an issue as to why a cervical X-ray series was recommended and performed if the MRI study was normal. It becomes even more complicated if the X-rays demonstrate intersegmental ligamentous instability in the flexion and extension views. Too often the MRI is used to rule out ligamentous injury, which it often will not demonstrate because the small ligamentous structures that stabilize the cervical segments are not well-demonstrated. Often only the stress of active weight-bearing motion will demonstrate the instability. Chiropractors and physicians who specialize in musculoskeletal disorders know this, but not all health care practitioners do.
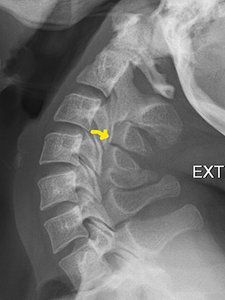
Case in point: A patient experienced ongoing pain in the neck radiating into the traps with intermittent headaches as a result of a whiplash injury from an auto accident eight months ago. The MRI was normal, as was the cervical spine study, except for intersegmental instability at the C3-4 motor unit, which indicates biomechanical hypermobility. This finding was not demonstrated on the MRI. (Figures 1-3)
Yes, it is possible to visualize a frank tear of the small intersegmental ligamentous structures on an MRI, but simple flexion and extension radiographs will demonstrate this type of intersegmental instability clearly, along with the biomechanical changes of associated articulations. There are MR units that can perform flexion and extension of the cervical spine and weight-bearing studies, but they are not generally available, are expensive, and the quality of the images may not be as good as the higher field strength units.1
Clinical Takeaway

As health care has evolved, patients are required to see their primary care physicians first more often than being able to initially see a specialist. This trend places more of a burden on the primary care physicians to diagnose and treat a wide spectrum of diseases. Often an MRI is ordered because the primary care physician believes it to be the most efficient diagnostic tool. It is what one might call the shotgun approach that increases the cost of health care.
As specialists in musculoskeletal disorders, we need to assess biomechanical changes that may be causing the patient's symptoms, and the most practical tool we have to do so is still radiography. As long as we use this modality prudently, we will not expose patients to unnecessary radiation. Cost issues aside, inappropriate imaging unnecessarily exposes patients to excessive radiation, inconvenience, and actual harms that come from the cascade of diagnostic and therapeutic interventions that often follow identification of a lesion that proves only to be an incidentaloma.
Reference
- Eurich MH. "Positional / Kinematic MRI of the Spine." Dynamic Chiropractic, July 16, 2007.