It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Abdominal Aortic Aneurysm and Low Back Pain
An aneurysm, by definition, is a sac formed by the dilatation of the wall of an artery, a vein or the heart. The chief signs of an arterial aneurysm are the formation of a pulsating tumor and often a bruit is heard over the swelling. Sometimes there are symptoms from pressure on contiguous parts.
The aorta is the largest artery in the body. It arises from the left ventricle, ascending and bending over the heart, descending anteriorly to the thoracic and lumbar vertebrae. It splits at L-4 into the common iliacs, femorals, tibials, and dorsalis pedis arteries, supplying the lower extremities. The average diameter of aorta is 2.0-2.5 cm. More than 90 percent of abdominal aneurysms are associated with atherosclerosis and can cause leg pain (claudication), numbness or fatigue. An artery may be sclerosed (hardened) but if the lumenal diameter isn't altered, there is no aneurysm.
Most abdominal aortic aneurysms do not produce symptoms, but some people feel a pulsating sensation in the abdomen. These silent (asymptomatic) aneurysms are often recognized by careful physical examination. Abdominal aortic aneurysm is most likely to occur in people older than 60 years, and it affects men more often than women.
Palpation of the femoralis, popiliteals and dorsalis pedis pulses will allow the examiner to quickly ascertain the quality of the arteries. I personally examine the dorsalis pedis pulses initially because they are the smallest and most distal palpable artery. If they are bounding normally, it generally indicates a clear channel is supplying the proper volume of blood to the feet. This test, when normal, helps differentiate a vascular from neurological lesion. This is important when performing an impairment rating or apportioning an impairment when coupled with your other clinical findings. Manual pressure on the toenail beds and a return to a pink color within three seconds is another quick vascular exam.
Vascular plethysmography, which is noninvasive, will identify the quality of the artery and quantity of blood flow to the lower extremities. Systolic blood pressures of both arms and legs using the standard blood pressure cuff or Doppler ultrasound coupling, utilizing the radial artery in the upper extremity and the posterior tibial artery in the lower extremity, is a good indicator of vascular health.
Blood pressures should be higher in the lower extremities; if inverted (the upper extremity blood pressures are higher than the lower extremity blood pressures), vascular disease should be suspected. The lowest acceptable level is if the upper and lower extremity blood pressures are equal.
S.N. Myer's Pressure Points: If lower varicose veins are present, press on the tibial bones. If painful, thrombophlebitis may be present and the blood pressure cuff should not be used because of a possible embolus creation.
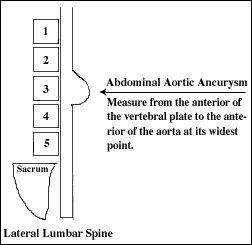
Aneurysms begin as micro tears and contain calcium and other blood coagulating material which seal the artery at the tear site. The greater number of arterial insults, tears, and bleeds will create more calcium to be laid down. Since calcium is radio-opaque, it can be visualized easily on x-ray. The routine x-rays taken are AP and Lateral, lumbar or abdominal views. The examiner looks at the lateral lumbar film and measures from the anterior of the lumbar or thoracic vertebra to the front of the aorta at the greatest posterior to anterior diameter. We measure from the front of the vertebra in question to the front of the aneurysm at that level. If the measuration is 4.0 cm or greater, that patient should be evaluated by a vascular physician prior to performing low back manipulation.
The pulsations of the aorta can rub against the anterior vertebral plates, causing erosion of the vertebra of vertebrae involved. This process also causes a thinning of the aorta at that level, making it more susceptible to rupture.
Palpation of an aortic aneurysm is possible in some cases. The exposed belly of the patient is palpated by the examiner. The patient's feet are flexed at the knees, the rectus abdominous muscle is relaxed and palpation is enhanced. The examiner gently pushes his/her fingers left and right of midline. With slow, steady pressure, the examiner will be able to almost reach the spine. If the aneurysm can be palpated right of midline, it needs a surgical evaluation. The aneurysm can cause low back pain due to the constant aortic pounding on the vertebral plate which is imbued with a rich supply of periosteal pain fibers.
The AP lumbar x-ray may also show an aneurysm. This should not be confused with a psoas muscle spasm, which will generally angulate the spine to the side of spasm. Fifteen percent of abdominal aortic aneurysms are not visible on x-ray.
As a side note, a renal artery aneurysm may also cause high blood pressure which should be suspected if the patient has back pain in addition to high blood pressure. Also, inner thigh pain in patients over 50 can be triggered by an aneurysm. A kidney punch test will help qualify if low back pain is of renal/ureter origin because shock waves from the "punch" will be felt into the groin area. Therefore, a urological referral may be necessary. Appropriate lab tests for inflammation/infection/stones and kidney function should be ordered. One study showed if a patient has hypertension and COPD with their aneurysm, there is a 90 percent chance of rupture within five years.
Remember an aneurysm can rupture at any time. If the patient ruptures while in your office, they need immediate hospitalization. If your screening and work up was performed prior to manipulation, you've helped to insulate yourself from a potential lawsuit, plus giving the patient a chance to receive care for the aneurysm.
I would like to acknowledge Dr. Michael Baron, radiologist, and Dr. Arthur Gresen, vascular surgeon, both of Las Vegas for providing the visual aids and technical help. Dr. Paul Williamson, MD, who wrote for Savage Laboratories, showed me how to palpate for abdominal aneurysms. I would also like to thank Richard Kraus, DC for his help.
Norman Engel, MS, DC, DABCO
Las Vegas, Nevada