It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
The Continuum of Care from Passive to Active Care
According to Janda there are predictable muscle imbalances present in most of our patients.1 Let's take a look at this hypothesis and see if it is reasonable and clinically applicable. Janda states that a sedentary lifestyle leads to an overuse of the postural, anti-gravity muscle systems. As a result shortening or tightness develops along predictable lines in muscles which "fight" to maintain static posture against gravity. These include such obvious muscles as the gastrosoleus complex, hamstrings, and upper trapezius. In contrast, other muscles have as their primary function to maintain stability during dynamic activities. Since we generally are working in constrained postures without much variety of movement, these dynamic stabilizers are underused and weaken or even atrophy. Examples include the gluteus medius which stabilizes the hip during the stance phase of gait and the lower trapezius which stabilizes the scapulothoracic joint during arm motions.
Denny-Brown one of the pioneering neurophysiologist of motor control studied muscle function in a similar way as Janda. He also discovered that muscle function was plastic. He studied birds who migrate long distances and compared them to birds who fly short distances.2 Interestingly, he found in birds who fly long distances their pectoralis muscles had more type 1 (short-twitch, tonic) muscle fibers, while the birds who flew shorter distances had more type 2 (fast-twitch, phasic) muscle fibers. Denny-Brown proved that structure follows function!
Janda by seeing how predictable muscle imbalances form in humans as a result of modern occupational repetitive strain simply applied Denny-Brown's understanding to a clinical situation. Now, we can quickly zero in on predictable muscle imbalances such as tight upper trapezius and weak lower trapezius and establish realistic goals to our rehabilitation program of relaxing/stretching the tight muscle and facilitating/strengthening the "weak link."
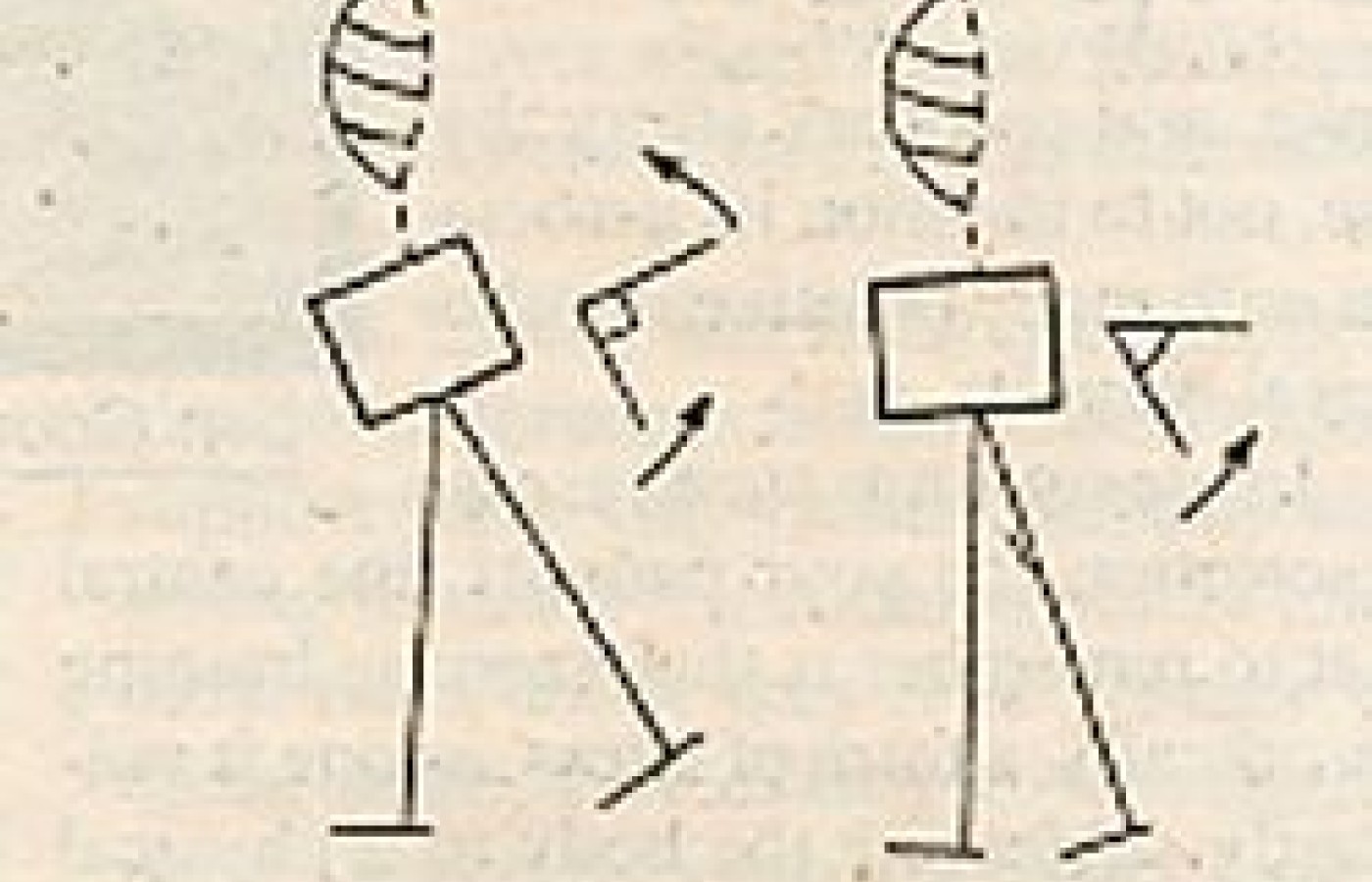
Janda's six movement pattern tests screen for the proper functioning of the majority of the clinically significant muscles we address.3 These tests are hip extension, hip abduction, trunk flexion, shoulder abduction, neck flexion, and the push-up. These tests are excellent tools for identifying the clinically relevant muscle imbalance. They also show whether or not a movement is being carried out with appropriate joint stability. For instance, if prone hip extension occurs at a fulcrum in the lumbar spine instead of in the hip joint it is a "false" hip extension and will lead to overstress of the lumbar zygapophyseal joints (see Figure 1 a&b). These tests are important because they drive treatment decision making. As Jerry Hyman says "they change what you do."

Figures adapted from Norris CM. Spinal stabilisation: muscle imbalance and the low back. Physiotherapy 1995: 81; 127-138.
Once we have identified a key muscle imbalance and altered movement pattern related to a specific pain generator then treatment can focus on the "key links" which are clinically most relevant in that patient. Treatment follows a continuum from passive to active care, which places progressively more responsibility on the patient.
STEP ONE: Adjust/Mobilize Stiff Joints
The initial treatment in restoring function to the locomotor system is to address joint hypomobility. According to Panjabi the joints are linked to the CNS by interneurons which act as transducers for signalling a problem.4 Their dysfunction can lead to treatment failure if soft tissue methods alone are employed. The muscles after all "react" to information provided by the osteoligamentous transducers.
STEP TWO: Relax/Stretch Tight or Overactive Myofascial Structures
It is crucial to check postural muscles for overactivity or tightness. These are the following muscles.
gastrosoleus QL hamstrings iliocostalis lumborum adductors upper trapezius piriformis levator scapulae TFL suboccipitals iliopsoas SCM rectus femoris scalenes If tightness or overactivity is found which relates to poor movement control then it should be relaxed or stretched. As an example if the quadratus lumborum is overactive during the stance phase of gait then it will substitute for the gluteus medius and lead to hip hiking and increased lateral shearing forces at the lower lumbar spine and sacroiliac regions. The hip abduction movement pattern will probably identify this by the presence of a "false" hip abduction occurring at the pelvis due to QL overactivity (see Figure 2 a&b).

Figures adapted from Norris CM. Spinal stabilisation: muscle imbalance and the low back. Physiotherapy 1995: 81; 127-138.
If the QL is not relaxed, then any exercise designed to strengthen the gluteus medius is likely to further overactivate the QL, thereby only reinforcing the muscle imbalance. This is one of Janda's most important clinical contributions. General strengthening exercises are unsuccessful unless they focus on the proper motor control. Inappropriate muscle activation will lead to a loss of proximal joint stability with resultant increased joint stress and eccentric muscle overload.5
STEP THREE: Motor Control (Neuromuscular Re-education)
Improving motor control has three aspects: 1) increasing the speed of contraction of primary joint stabilizers. This is facilitated by propriosensory exercises on labile surfaces. The use of unexpected pushes also helps develop this stabilization function; 2) the kinaesthetic awareness to perform movements with the proper muscle activation or co-contraction. Specific advice, patient pre-positioning, verbal commands, and proprioceptive cues are used to facilitate this; 3) training the endurance of static proximal stabilizers. The lower trapezius, for example, should be trained to maintain a tonic contraction throughout dynamic arm motions. This endurance is trained with exercises of <50 percent MVC which are carried out slowly to selectively activate type I, tonic muscle fibers.6 Five to 10 second isometric holds may also be incorporated.
The key proximal muscle stabilizers of dynamic activity are:
- lower traps
- serratus anterior
- deep neck flexors
- latissimus dorsi
- multifidus/transverse abdominus
- gluteus medius
- gluteus maximus
- vastus medialis oblique
STEP FOUR: Dynamic strength and endurance (torque production ability)
This is the last step in training. It includes mass movements which require distal mobility (steps 1 & 2) with proximal stability (step 3). These exercises are carried out isotonically or isokinetically at >80 percent of MVC to selectively train type II (phasic) muscle fiber function. The muscles which should be trained to their threshold/overload are:
- rectus abdominus
- gluteus maximus
- quadriceps
- deltoid
- latissimus dorsi
- rotator cuff muscles
When training patients it is important to recall that most injuries are a result of a sudden, unexpected perturbation not a gross trauma, thus motor control not strength is the key to injury prevention. Bogduk and Twomney say: "Such processes may underlie what might otherwise be called 'fatigue' in a ligament or capsule. After prolonged strain, ligaments, capsules, and intervertebral discs of the lumbar spine may creep, and they may be liable to injury if sudden forces are unexpectedly applied during their vulnerable, recovery phase."7 Cholewicki and McGill say, "Clinicians need to explore the effectiveness of motor control training as an adjunct to the muscle strength improvement for reducing low back pain episodes."
References
- Janda V. On the concept of postural muscles and posture in man. Aus J Physioth 1983;29:83-84.
- Denny-Brown D. The histological features of striped muscle in relation to its functional anatomy, Proceedings of the Royal Society of London 1929;104B: 371-411.
- Janda V. Evaluation of muscle imbalance. In: Liebenson C (ed) Spinal Rehabilitation: A Manual of Active Care Procedures. Williams and Wilkins, Baltimore 1996.
- Panjabi MM. The stabilizing system of the spine. Part 1. Function, dysfunction, adaptation, and enhancement. J Spinal Disorders 1992;5:383-389.
- Edwards RHT, Jones DA, Newham DJ, Chapman SJ. Role of mechanical damage in pathogenesis of proximal myopathy in man. Lancet 1984; March 10:548-551.
- McArdle WD, Katch FI, Katch VL. Exercise Physiology, Energy, Nutrition and Human Performance, 3rd ed. Lea Febiger, Philadelphia ch 20. 1991; p 384-417.
- Cholewicki J, McGill SM. Mechanical stability of the in vivo lumbar spine: implications for injury and chronic low back pain. Clin Biomech 11:1;1-15, 1996.
Craig Liebenson, DC
Los Angeles, California