It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
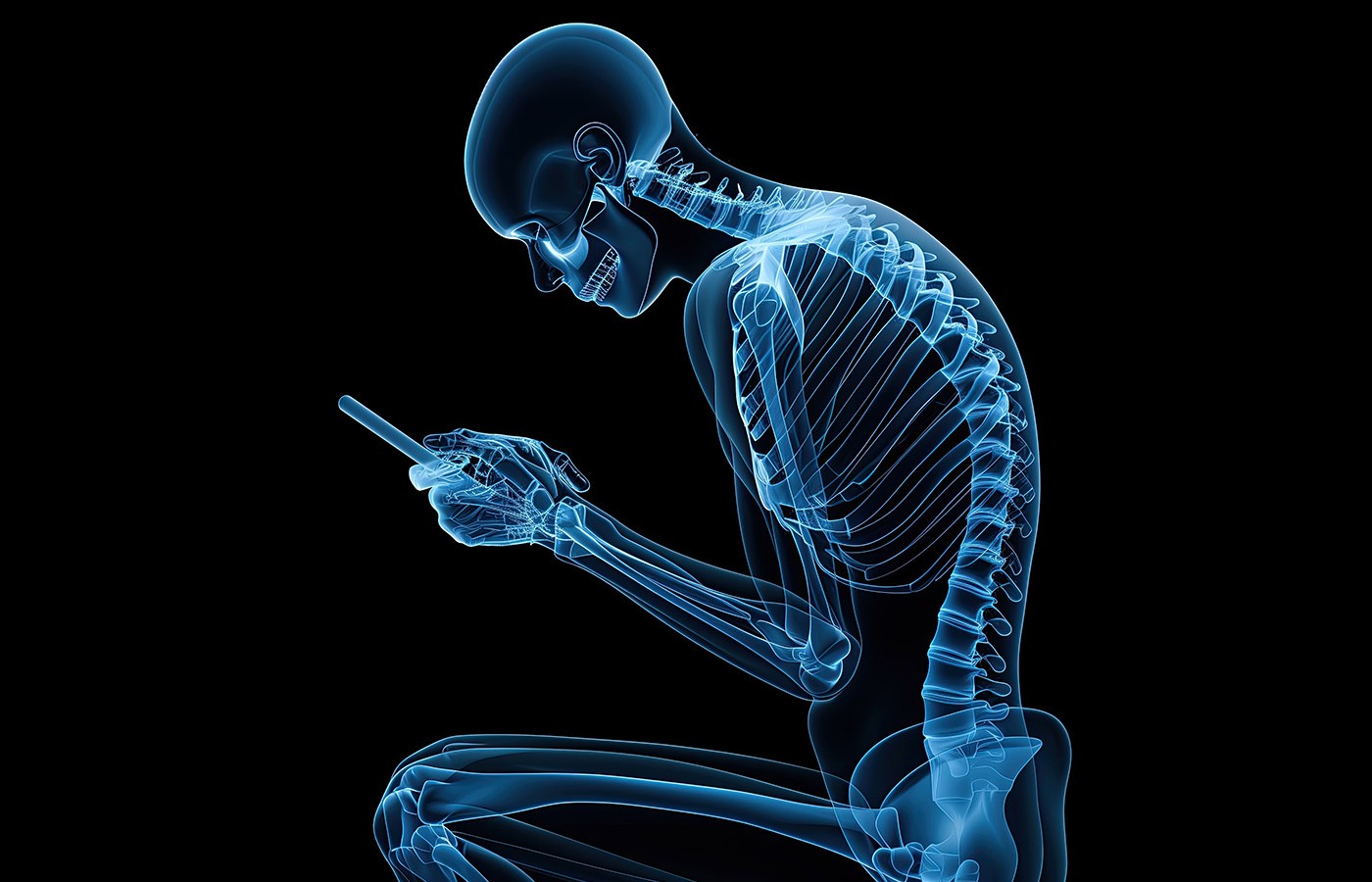
Forward-Head Posture: Not Just an MSK Issue
Corticomuscular coherence (CMC) is a widely used measure of how brain and muscle electrical activities synchronize – how brain activity in the motor cortex syncs with muscle activity. Increased CMC in patients with forward-head posture (FHP) suggests postural misalignment impacts much more than just the musculoskeletal system.
A new prospective case-control study involving 64 adults (ages 18-25 and free of musculoskeletal symptoms) assessed FHP using the craniovertebral angle, yielding two groups: NHP (normal head posture; CVA greater than 50 degrees) and FHP (CVA less than 50 degrees).
The research team then evaluated balance using a plate-based balance system that subjected study participants to four progressively challenging conditions: standing with eyes open, standing with eyes closed, unstable standing with eyes open, and unstable standing with eyes closed. During all four scenarios, EEG and EMG signals were acquired simultaneously to evaluate corticomuscular coherence in five frequency bands (Hz): delta, beta, theta, alpha, and gamma.
Results: “A post-hoc analysis revealed significant differences between the FHP and NHP group, in terms of peak CMC, average CMC, and the five frequency bands. … Additionally, it further confirmed that those differences were most apparent at a higher difficulty level, particularly stage 4, and occasionally stage 3.” Subjects with forward-head posture displayed increased CMC during the balance tasks, suggesting compensatory cortical recruitment was needed to maintain balance / stability.
Conclusion: “Our findings align with previous studies that highlight the increased cortical demand associated with postural misalignment and task complexity. However, differences in neural strategies under cognitive versus biomechanical load suggest that FHP places a unique compensatory burden on the brain, particularly during physically challenging tasks.
“Clinically, these findings underscore the importance of early postural interventions to alleviate neural and biomechanical inefficiencies, thereby improving patient outcomes and reducing the risk of chronic pain.”
Source: Anwar G, et al. Comparison of corticomuscular coherence under different balance paradigms in individuals with and without forward head posture. Sci Rep, 2025;15:22985 (open access: Read Here).