New York's highest court of appeals has held that no-fault insurers cannot deny no-fault benefits where they unilaterally determine that a provider has committed misconduct based upon alleged fraudulent conduct. The Court held that this authority belongs solely to state regulators, specifically New York's Board of Regents, which oversees professional licensing and discipline. This follows a similar recent ruling in Florida reported in this publication.
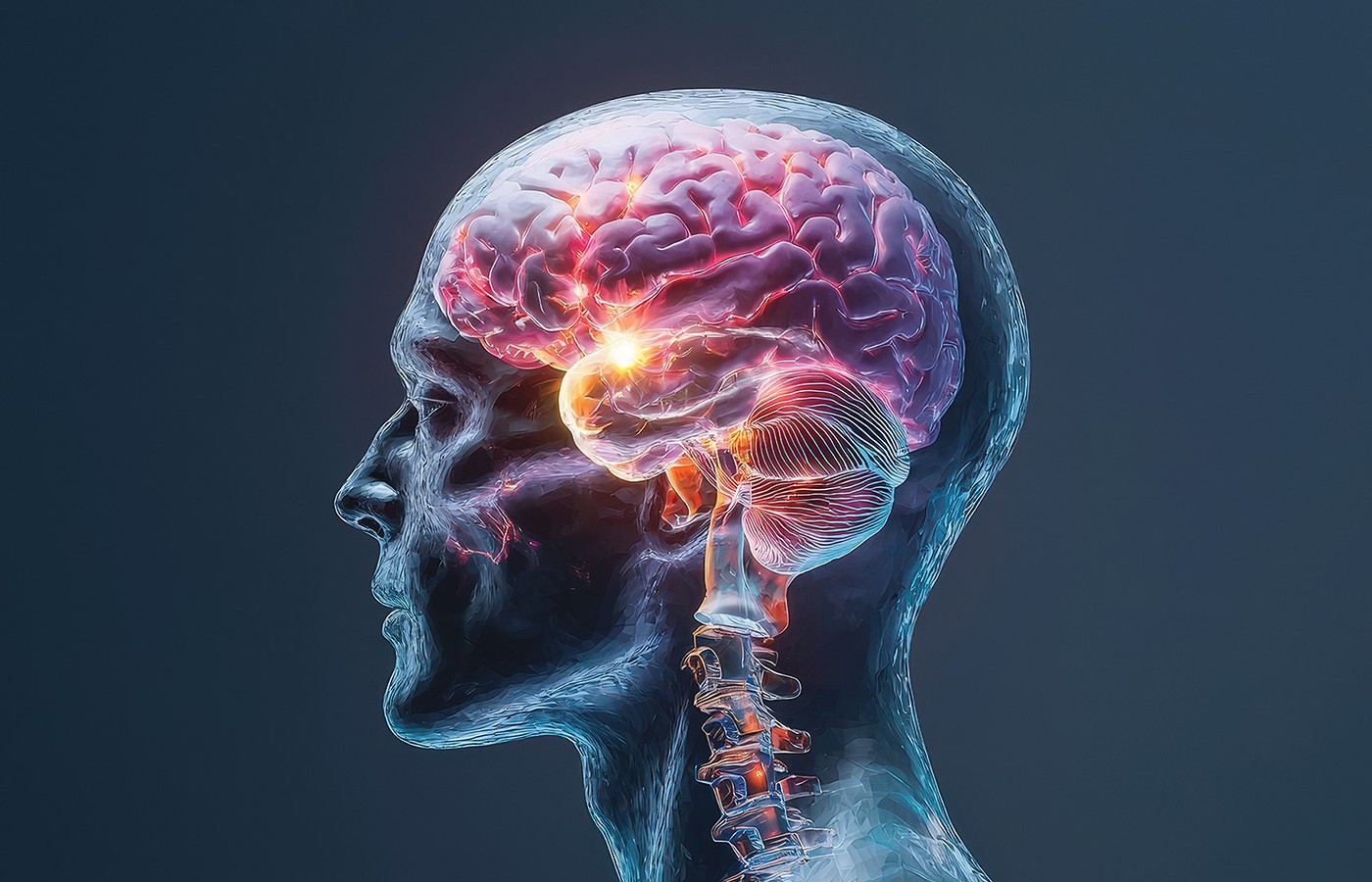
From Sciatica to Brain Tumor: A Life-Saving Diagnosis
- A 42-year-old male former patient arrives at your chiropractic office with excruciating low back pain that travels all the way down his right leg to his foot; headaches; and nausea.
- A positive Babinski sign, accompanied by ankle clonus, clearly indicates that upper-motor neurons are involved, requiring immediate referral to a specialist for advanced imaging.
- The patient was diagnosed with a glioma grade II after an MRI and biopsy: a slow-growing brain tumor with cells that divide slowly.
A 42-year-old male former patient arrives at your chiropractic office with excruciating low back pain (7/10) that travels all the way down his right leg to his foot (9.5/10). According to him, the pain is scorching and severe, and it gets worse when he sits for a long time or coughs. Additionally, the patient states that he has had headaches and nausea, which he never experienced before.
He claims that although he has experienced sporadic low back pain for the past 10 years, this episode is more severe and has not gotten better with time. It is similar to the pain he had about two years ago, when he first presented at your clinic.
At that time, a spinal surgeon had recommended surgery to correct an MRI-confirmed disc herniation (sequestration) at L5. But the patient instead chose your treatment package, which included spinal manipulation, manual therapy, laser, and rehabilitation. After two months of care, the patient was discharged with little back pain (2/10), no leg pain (0/10), and good function, and was good-to-excellent on lumbar physical performance tests. You discharged him and instructed him to continue with physical endurance activities at home.
You now perform a full examination with the following findings:
- Physical Examination: Evaluation of posture and movement elicits painful lumbar flexion and antalgic tilt to the left.
- Physical Performance Test: Poor endurance of the lumbar muscle groups. His performance is below the mean on all tests. The patient had stopped engaging in physical endurance activities.
- Neurological Examination: L4-S1 dermatomal paresthesia and weakening on the right side, particularly in the right foot’s dorsiflexion.
- Reduced Achilles reflex on the right leg.
- Bilateral ankle clonus.
- Straight leg positive elevated at 30 degrees with worsening radicular symptoms.
- Bilateral Babinski sign is positive.
- No bladder or bowel issues at the moment.
Clinical Challenge
Given the positive Babinski sign with ankle clonus, what is your next step?
- Repeat previously successful treatment package, which included spinal manipulation, manual therapy, laser, and rehabilitation.
- Send the patient to the emergency room for an MRI and neurosurgical consultation to evaluate for significant neurological compromise.
- Administer lumbar decompression treatment and track the development of symptoms.
Discussion / Learning Points
Some chiropractors may automatically think back to the previous successful treatment package on any given patient. They may think that the neurological symptoms will resolve with time and therapy. But a positive Babinski sign, accompanied by ankle clonus, clearly indicates that upper-motor neurons are involved, which raises concerns for a serious problem. This requires immediate referral to a specialist for advanced imaging.
Although conservative treatment is effective for many lumbar disc herniations, including disc sequestrations, the warning signs in this case call for escalation.1-3 A positive Babinski sign with ankle clonus means the central nervous system is malfunctioning. This could be due to a brain tumor, spinal-cord compression, multiple sclerosis, or some other illness. This is a red flag (in contrast to peripheral radiculopathy).
The best evidence-based course of action is option B, which involves an ER MRI and a referral for a neurosurgical consultation. In this situation, postponing proper diagnosis could result in irreversible damage. Time is of the essence. This is not a time when you can send the patient for an MRI at your local radiology center in two weeks. If this is a brain tumor, it could be a glioblastoma, which is fast-growing.
This patient was diagnosed with a glioma grade II after an MRI and biopsy. A grade II glioma is a slow-growing brain tumor with cells that divide slowly, which means it has a more favorable prognosis than a glioblastoma.
This case is a sobering reminder that while conservative care can be highly effective, it is not always the right solution – especially when neurological red flags emerge. The presence of a positive Babinski sign and ankle clonus demanded immediate action, and delaying further investigation could have led to irreversible consequences. In this instance, swift action led to an early diagnosis of a brain tumor, offering the patient a fighting chance. Vigilance saves lives.
References
- Chiu CC, Chuang TY, Chang KH, et al. The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clin Rehabil, 2015;29:184-95.
- Kasch R, Truthmann J, Hancock MJ, et al. Association of lumbar MRI findings with current and future back pain in a population-based cohort study. Spine, 2022;47:201-211.
- Panagopoulos J, Magnussen JS, Hush J, et al. Prospective comparison of changes in lumbar spine MRI findings over time between individuals with acute low back pain and controls: an exploratory study. Am J Neuroradiol, 2017;38:1826-1832.