It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Understanding the Risks of Anticholinergic Drugs
- Anticholinergic drugs work by blocking the action of acetylcholine, a crucial neurotransmitter involved in memory and muscle control.
- Despite their common use for ailments like allergies, insomnia, overactive bladder, and depression, especially prevalent among seniors, their prolonged use can detrimentally affect cognitive function and balance.
- The Anticholinergic Burden Calculator offers a valuable tool for assessing the cumulative impact of anticholinergic medications on cognitive function.
Editor's Note: This article appeared originally in Acupuncture Today, DC's sister publication.
In the profitable world of modern health care and “polypharmacy,” certain medications, while potentially beneficial in treating various conditions, may harbor unforeseen dangers. Among these are anticholinergic drugs, which not only increase the risk of falls, but are also associated with the development dementia, particularly in older adults.
Recognizing the risks posed by this class of medications is vital for health care practitioners who can advocate for their patients to explore natural alternatives (in consultation with their primary care physicians). Additionally, using tools such as the Anticholinergic Burden Calculator can assist in evaluating and mitigating the cognitive impact of anticholinergic drugs.
Working with seniors at an independent/assisted living community with a memory unit, I witness firsthand the consequences of years of taking this class of drugs, and it’s not pretty.
Association With Dementia
Anticholinergic drugs work by blocking the action of acetylcholine, a crucial neurotransmitter involved in memory and muscle control. Despite their common use for ailments like allergies, insomnia, overactive bladder, and depression, especially prevalent among seniors, their prolonged use can detrimentally affect cognitive function and balance, leading to increased mortality rates.
Numerous studies have underscored the compelling link between anticholinergic drug use and dementia. A study in JAMA Internal Medicine revealed that long-term use of anticholinergic drugs was associated with a significantly higher risk of dementia, with the risk escalating with higher cumulative doses of these medications.1
Another study in the British Medical Journal echoed these findings, emphasizing the necessity for cautious prescribing and monitoring, particularly among older populations.2 Additionally, a Harvard Health blog highlighted a 54% higher risk of dementia associated with taking anticholinergics for the equivalent of three years or more, compared to a three-month duration.3
The mechanisms underlying the association between anticholinergic drugs and dementia are complex and not yet fully understood. However, it is believed that inhibition of acetylcholine receptors in the brain may contribute to the accumulation of amyloid plaques and neurofibrillary tangles, characteristic hallmarks of Alzheimer’s disease and other forms of dementia.
Evaluating Cost vs. Benefit
Given the potential risks associated with anticholinergic drugs, health care professionals must evaluate their benefits against cognitive effects, particularly in older patients who may be more susceptible to complications.
The Anticholinergic Burden Calculator offers a valuable tool for assessing the cumulative impact of anticholinergic medications on cognitive function. By inputting a patient’s medication list, health care professionals can generate an “anticholinergic burden score,” aiding in clinical decision-making. Figure 1 is the output given two common drugs and the output of the calculator.
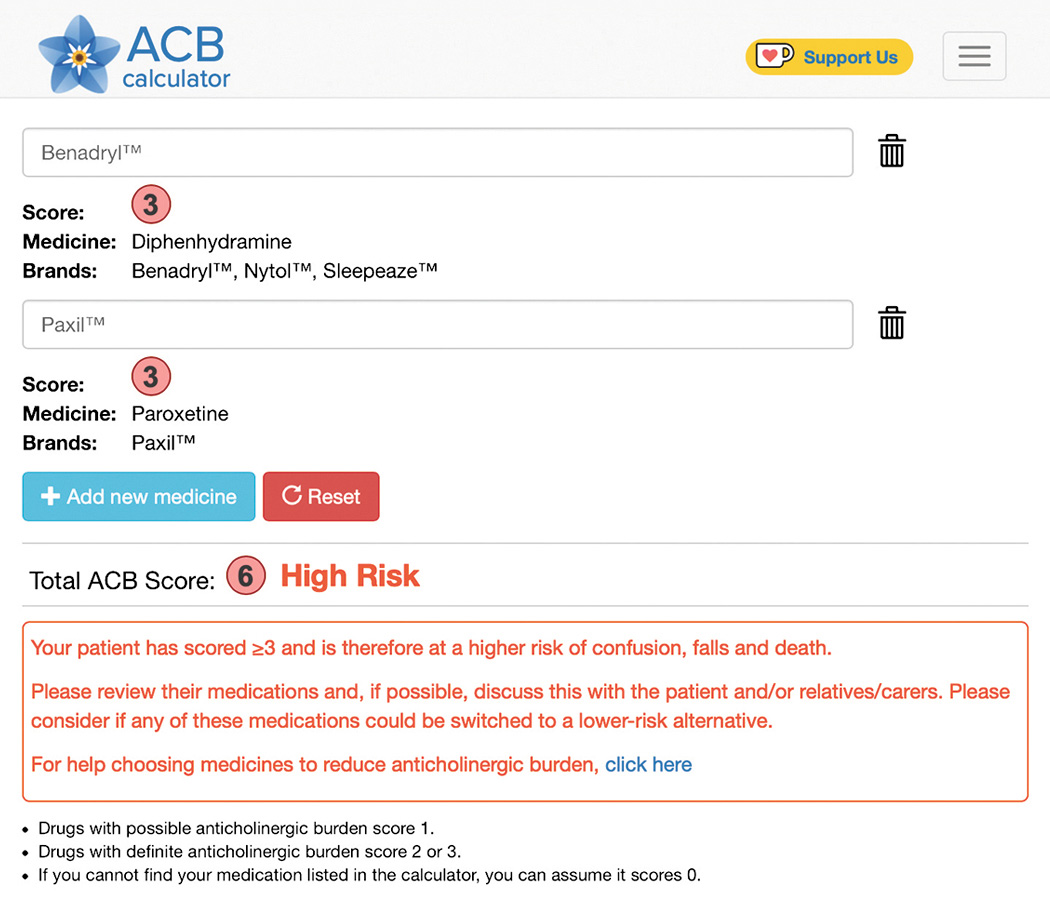
The Anticholinergic Burden Calculator can provide you with an evidence-based printout to help communicate with your patient’s health care provider(s), fostering informed discussions about the potential risks and benefits of specific medications. Armed with objective data from the calculator, we can also educate patients about the importance of medication management and empower them to make informed decisions about their health care.
Safer Alternatives
Safer alternatives exist for common conditions treated with anticholinergic drugs. For instance, allergies can be managed with quercetin and bromelain,4 while anxiety and depression may respond to 5-HTP, L-tryptophan, L-theanine, St. John’s wort, folate or dehydroepiandosterone (DHEA).5 Insomnia can be addressed with CBD, L-theanine, melatonin, valerian, kava kava, chamomile, skullcap or lemon balm.6
Notably, acupuncture and traditional Chinese herbal medicine offer safe and effective treatment options for these conditions without resorting to brain-damaging anticholinergic medications.
Speaking of brain damage, Alzheimer’s disease is on the rise in the U.S. from the current estimate of 5.8 million to a whopping 14 million Americans predicted by 2060.7-8 For patients with minor dementia or Alzheimer’s, incorporating medium-chain fatty acids (MCT oil) into their diet, at a recommended dosage of two tablespoons per day, may yield notable improvements.9
Clinical Pearls
The dangers of anticholinergic drugs in potentially leading to dementia underscore the importance of vigilant medication management and risk assessment in clinical practice. Tools like the Anticholinergic Burden Calculator offer invaluable support in identifying and mitigating the cognitive risks associated with these medications.
References
- Coupland CAC, Hill T, Dening T, et al. Anticholinergic drug exposure and the risk of dementia: a nested case-control study. JAMA Intern Med, 2019;179(8):1084-1093.
- Gray S L, Hanlon J T. Anticholinergic drugs and dementia in older adults BMJ, 2018;361:k1722.
- Common anticholinergic drugs like Benadryl linked to increased dementia risk. Harvard Health, Jan. 19, 2022.
- Asher BF, Seidman MD, Reddy WD, Omole FS. Integrative medical approaches to allergic rhinitis. Curr Opin Otolaryngol Head Neck Surg, 2015 Jun;23(3):221-5.
- Larzelere MM, Wiseman P. Anxiety, depression, and insomnia. Prim Care, 2002 Jun;29(2):339-60, vii.
- Botanical Medicines to Support Health Sleep and Rest. U.S. Department of Veterans Affairs.
- Matthews KA, Xu W, Gaglioti AH, et al. Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015-2060) in adults aged ≥65 years. Alzheimers Dement, 2019;15(1):17-24.
- Alzheimer’s disease facts and figures. Alzheimers Dement, 2019;15(3):321-87.
- Reddy B. “Losing your Mind? Try Coconut Oil.” Acupuncture Today, January 2017.



