It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
When to Use Pain Neuroscience Education
In my last article [April issue], I discussed using pain neuroscience education (PNE) with chronic pain patients. More discussion is beneficial about phenotyping the pain our patient presents with to better determine when to use PNE.
PNE is a broad category of education and therapies that address maladaptive neuroplasticity of the CNS in chronic pain patients. Its purpose is to rewire or retrain the brain to interpret normal afferent signals as normal and not as pathological alarms of danger or damage. The first step is to educate patients about the changes in their brain in chronic pain, then use a variety of therapies to make corrections.
PNE and Chiropractors
In studies done in North America (80.6%), Australia (93.5%) and the Netherlands (91%), chiropractors are aware that psychosocial factors affect patients and their outcomes. However, a majority have not identified appropriate techniques to manage these factors and lack the confidence in doing so.
Each type of pain requires a different approach to care, and PNE is not useful for all types of pain; it is meant for nociplastic pain. So first, you must triage your patient.
Types of Pain
Nociceptive pain is defined as pain arising from actual or threatening damage (i.e., chemical, mechanical or thermal) to non-neural tissue and is due to the activation of nociceptors, transmitted by polymodal A-delta and C fibers in skin, bone, connective tissue, discs, muscles and viscera.
Neuropathic pain is pain caused by injury to or dysfunction of the peripheral and/or central nervous system in the absence of direct nociceptive input.
Nociplastic pain or central sensitization is defined as an amplification of neural signaling within the CNS that elicits pain hypersensitivity. CS is an umbrella term of a constellation of dysfunctions, like inflammation, within the CNS that all contribute to decreasing the threshold for pain, more reactive to various stimuli not necessarily directly linked to pain in normal function (e.g., psychosocial factors such as stress, emotions, behavior) and result in an increased perception pain.
To be clear, this pain is real to the patient and demonstrable on fMRI, just out of proportion of or lack of physical damage. Current research shows nociplastic pain is often associated with or triggered by psychosocial events or factors.
Mixed pain is what it sounds like; a patient can have a mixture of pathology going on to cause their S/S. They could have nociceptive and neuropathic pain sources, or nociceptive or neuropathic pain can lead to nociplastic in cases of chronic pain, or whiplash syndrome, as examples.
Please see the resources listed below as the source for these definitions and phrasing. I strongly recommend you check out articles on related topics in this publication by DiDuro, Seaman, Murphy, Hammer, Heller, and Rosner – names known to all of us.
Chiropractors need no primer on diagnosing pain. However, I want to highlight a paper that helped me with this process: “Applying Modern Pain Neuroscience in clinical Practice: Criteria for the Classification of Central Sensitization Pain,” by Jo Nijs, et al. They break this phenotyping of pain down into two steps and three criteria, all in a nice-to-follow algorithm. (See figure below)

Step 1: Exclude or diagnose neuropathic pain.
Step 2: Exclude or diagnose CS using 3 criteria:
- Disproportionate pain experience?
- Diffuse pain distribution?
- Hypersensitivity of senses unrelated to MSK system (Central Sensitization Inventory >40?)
CS is often present in various chronic NMSK conditions, including chronic whiplash syndrome, IBS, chronic low back pain, shoulder impingement, fibromyalgia, and others. It is important to remember that not all chronic pain is nociplastic, and several S/S on the nociplastic list (e.g. responsive to weather changes or no known medical pathology) have known causes to NMSK providers and chiropractors, but apparently not to behavioral health providers (see the book The Way Out by Alan Gordon, an otherwise excellent book).
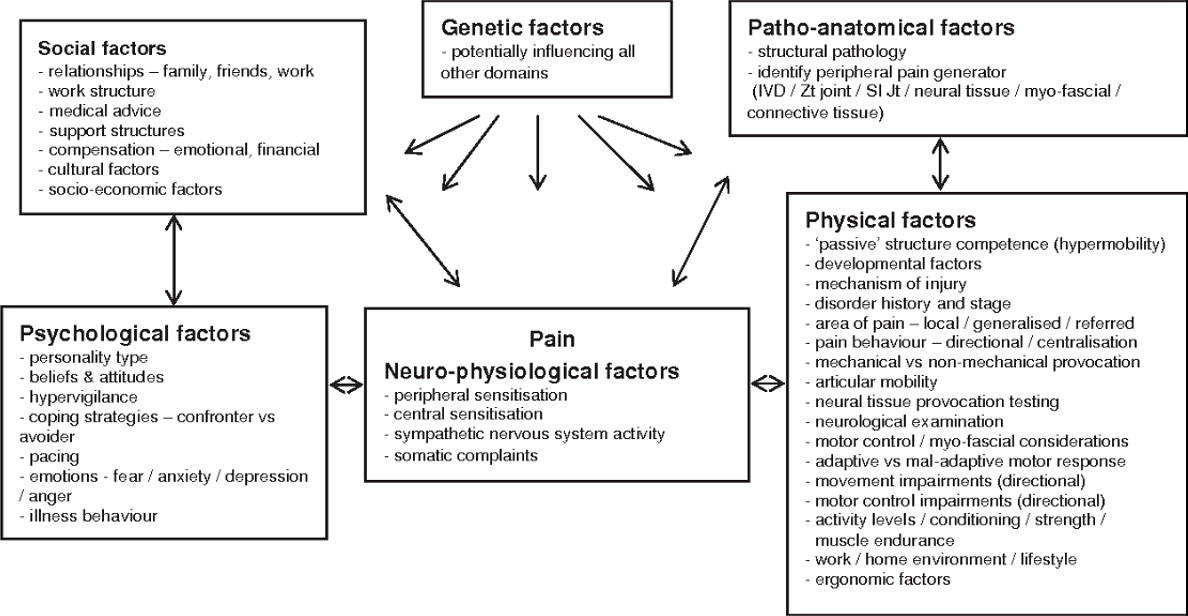
That is not to say that they do not contribute to the nociplastic picture, but not a mystery to be ignored, either, like joint dysfunction often is, for example. But many factors contribute to cause nociplastic pain in some patients. (See figure below)
Another frequently not recognized sign of maladaptive neuroplasticity contributing to the patient presentation is the adjustments not holding when reasonably expected to be stabilizing.
A word about the Central Sensitization Inventory questionnaire. In recent studies, its value has been questioned and shown it is mostly sensitive for psychological factors of chronic pain.
Exclusions for use of PNE include pain from cancer, autoimmune disorders, clearly diagnosed neuropathic pain, and some arthritis conditions. Not that PNE cannot help these patients with coping, but reduction or resolution of pain is not as reasonable an expectation. When in doubt, try.
Resources
- Nijs J, Torres-Cueco R, van Wilgen CP, Girbes EL, et al. Applying modern pain neuroscience in clinical practice: criteria for the classification of central sensitization pain. Pain Physician, 2014 Sep-Oct;17(5):447-57.
- O'Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther, 2005 Nov;10(4):242-55.
- Nijs J, De Baets L, Hodges P. Phenotyping nociceptive, neuropathic, and nociplastic pain: who, how, & why? Braz J Phys Ther, 2023 Jul-Aug;27(4):100537.
- Nijs J, Malfliet A, Nishigami T. Nociplastic pain and central sensitization in patients with chronic pain conditions: a terminology update for clinicians. Braz J Phys Ther, 2023 May-Jun;27(3):100518.
- Haanstra T, Miller J. Dutch chiropractors’ perceptions on including psychosocial factors in the evaluation and management of patients: a survey. Clin Chiro, 2011;14:112-121.
- Bennett EE, Walsh KM, Thompson NR, Krishnaney AA. Central Sensitization Inventory as a predictor of worse quality of life measures and increased length of stay following spinal fusion. World Neurosurg, 2017 Aug; 104:594-600.
- Neuropathic Low Back Pain: Where Does It Hurt? | Dynamic Chiropractic - DiDuro
- Understanding and Diagnosis of Nerve-Related Pain | Dynamic Chiropractic - Heller



