On Oct. 21, 2025, a judge in Florida issued a groundbreaking decision in Complete Care v State Farm, 25-CA-1063. It concerns a fact pattern that many chiropractic doctors have faced wherein an insurer, such as State Farm or Allstate, decides to simply stop paying all claims submitted by a healthcare provider.
| Digital ExclusiveUnderstanding Peripheral Neuropathy
Peripheral neuropathy (PN) is a complex and poorly understood condition in which the body’s peripheral nerves gradually deteriorate. Symptoms associated with this condition range from mild tingling and numbness to severe throbbing, stabbing and/or burning pain. Intense nerve pain affects as many as two-thirds of people afflicted with peripheral neuropathy and the symptoms are notoriously difficult to treat.
Unfortunately, peripheral neuropathy is surprisingly common, affecting 10% of middle-aged adults and nearly 40% of people over the age of 70.1
While any peripheral nerve may be involved, the sensory nerves that go to the feet are the most prone to developing neuropathy. Part of the reason these nerves are preferentially targeted is because they are so long; a single nerve that goes to the bottom of the foot can be over 3 feet long, and the nerve’s axon can be 20,000 times longer than the cell body.2
Because the cell body assists with nourishing and maintaining the axon, providing nutritional and metabolic support to such a long structure can be difficult under ideal conditions. The connection between nerve length and peripheral neuropathy is evidenced by the fact that tall people are significantly more likely to get neuropathy than their shorter peers.3
Some of the more common causes of this disease include various autoimmune disorders, alcoholism, kidney disease, exposure to toxins, vitamin deficiencies, and certain medications. Chemotherapy drugs are notorious for producing peripheral neuropathy.
While all of these conditions increase the risk of neuropathy, far and away the greatest risk factor for developing peripheral neuropathy is diabetes. An estimated 20 million Americans currently have diabetes-related neuropathy, and that number is expected to double as more Americans develop pre-and type 2 diabetes.4
According to Feldman, et al.,5 the neuropathic complications associated with diabetes places a tremendous burden not just on individuals affected, but also society as a whole. The authors emphasize that there is a pressing need to understand the cellular mechanisms responsible for the development of diabetic neuropathy in order to develop drugs that can effectively treat and prevent this disabling condition.
Unfortunately, despite 50 years of intense research, pharmacological interventions for peripheral neuropathy remain relatively ineffective.5
Exercise Interventions
Because pharmacological interventions have been unable to appreciably improve the quality of life for those suffering with peripheral neuropathy, researchers have begun focusing on alternative treatments, such as exercise,6 nerve glide stretches,7 vibration therapy,8 and nutrition.9 Of these interventions, exercise interventions have been studied most extensively.
In one of the first papers to evaluate the efficacy of exercises in the management of peripheral neuropathy, researchers from the University of Kansas had 17 peripheral neuropathy patients perform a 10-week program of aerobic and strengthening exercises.6 At the start and stop of the study, the authors evaluated pain levels using visual analog scales, performed nerve conduction velocities, and measured the density and branching patterns of cutaneous nerves located in skin taken from biopsies.
Participants performed light aerobic exercises on devices such as elliptical trainers and bicycles, and did a conventional strengthening protocol targeting all of the major muscle groups. The exercises were performed at a moderate intensity.
At the end of the 10-week study, the exercise group experienced significant reductions in pain and neuropathic symptoms, and they actually grew additional cutaneous nerve fibers following the intervention. This latter finding was consistent with prior research confirming that exercise can increase the number of sensory nerve fibers present in the skin,10 which is important, as the regeneration of cutaneous nerve fibers correlates with improved clinical outcomes.11
The findings of these early research studies have been corroborated by more recent research confirming that exercise interventions can delay both the onset and progression of diabetes and diabetes-related peripheral neuropathies.12-20 Exercise intervention has also been proven to be effective when managing chemotherapy-induced peripheral neuropathy.21-22
One study found that just eight weeks of resistance and balance training produced statistically significant reductions in patient-reported pain, dynamic balance, range of motion, and quality of life in cancer survivors.22
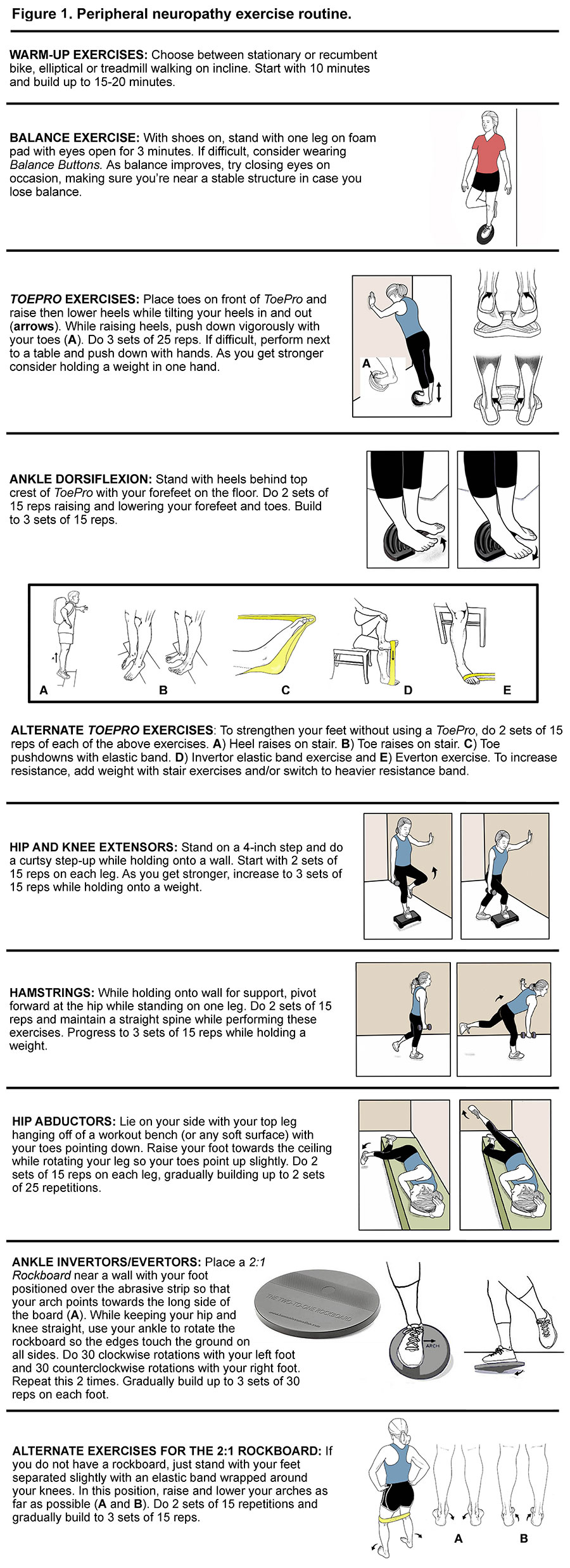
The positive effects of exercise have been related to improved glycemic control, increased blood flow, enhanced neurotrophic support and suppression of pro-inflammatory responses. According to Holmes, et al.,23 a combination of aerobic and strength training gets the best results, and my favorite program is outlined in Figure 1.
In addition to exercise, gentle nerve glide stretches have also been shown to improve nerve function in people with neuropathy. Performing range-of-motion and specific nerve glide stretches just 3 times daily for 10 minutes appreciably reduced nerve pain while improving strength and sensation in patients suffering from chemotherapy-induced peripheral neuropathy.24 (Figure 2)
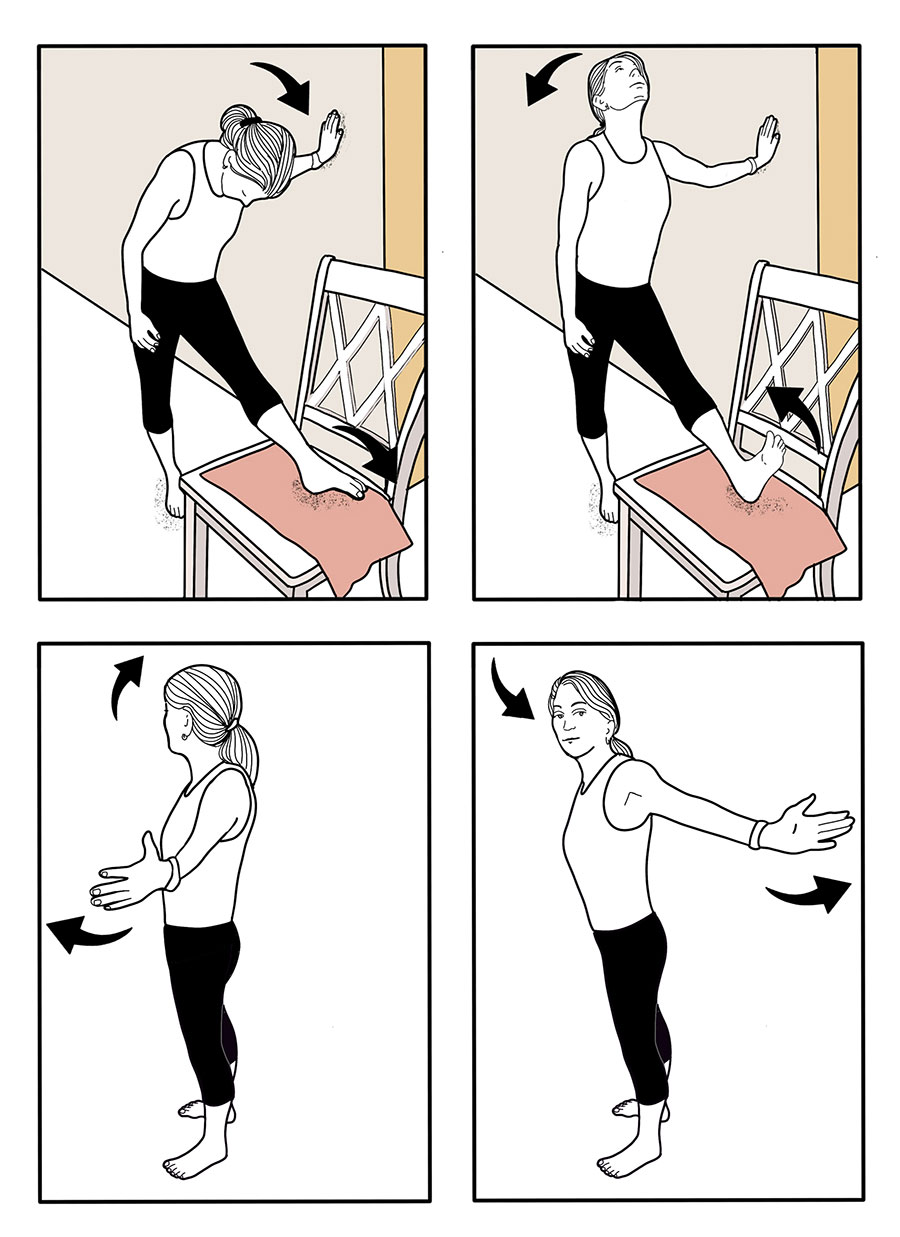
The authors claim that nerve glide exercises improve nerve function by decreasing neural edema as stretching the nerve enhances axoplasmic flow. Other authors speculate that nerve glide techniques work because they loosen adhesions that restrict proper nerve motion.
Regardless of the mechanisms, gently moving peripheral nerves back and forth can reduce pain and improve function. In fact, many of the exercises in the peripheral neuropathy strengthening program were included because they mobilize branches of the sciatic nerve, such as the tibial and superficial peroneal nerves, which are the longest nerves in the body and are almost always affected by peripheral neuropathy.
Clinical Pearls
Given the diverse mechanisms responsible for the development of peripheral neuropathy, it is clear that alternative interventions can play a pivotal role in the management of this complex and often painful condition. Unlike many pharmacological interventions, alternative interventions such as exercise and nerve glide mobilizations are safe, effective, and inexpensive. Research shows these techniques can reduce pain, enhance balance, and improve the overall quality of life for those afflicted with this painful condition.
People dealing with this difficult condition deserve efficacious alternate treatment approaches, because according to Feldman, et al.,5 “All clinical trials aimed at altering the progressive course of diabetic neuropathy have failed.” The authors go on to state: “Large pharma has now walked away from diabetic neuropathy as a result of our lack of a basic understanding of the disease, whereas the enormity of the problem has reached epidemic proportions. The societal costs are only dwarfed by the individual cost to each patient that include pain and inability to work along with poor quality of life.”
Given that these statements come from some of the world’s leading experts on pharmacological management of peripheral neuropathy, it’s time to start focusing on alternative therapies, particularly exercises, stretches, and nutritional interventions.
References
- Hicks C, Wang D, Windham B, et al. Prevalence of peripheral neuropathy defined by monofilament insensitivity in middle-aged and older adults in two US cohorts. Scientific Rep, 2021;27;11:19159.
- Wang J, Medress Z, Barres B. Axon degeneration: molecular mechanisms of a self-destruction pathway. J Cell Biol, 2012;196:7-18.
- Kote G, Bhat A, Thajuddeen K, et al. Peripheral insensate neuropathy-is height a risk factor? J Clin Diag Res, 2013;7:296.
- Menke A, Casagrande S, Geiss L, et al. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA, 2015;314:1021-1029.
- Feldman EL, et al. New horizons in diabetic neuropathy: mechanisms, bioenergetics, and pain. Neuron, 2017:1296-1313.
- Kluding PM, et al. The effect of exercise on neuropathic symptoms, nerve function, and cutaneous innervation in people with diabetic peripheral neuropathy. J Diabetes and Its Complications, 2012;26.5:424-429.
- Hammond E, Pitz M, Steinfeld K, et al. An exploratory randomized trial of physical therapy for the treatment of chemotherapy-induced peripheral neuropathy. Neurorehab Neural Repair, 2020;34:235-246.
- Sabziparvar M, Naghdi S, Ansari N, et al. Local plantar vibration for the treatment of diabetic neuropathy: a case report. J Diabetes Metab Disord, 2021;20:2115-2119.
- Ziegler D, Nowak H, Kempler P, et al. Treatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: a meta-analysis. Diabet Med, 2014 ;21:114-121.
- Smith AG, et al. Lifestyle intervention for pre-diabetic neuropathy. Diabetes Care, 2006;29:1294-1299.
- Baskozos G, et al. Molecular and cellular correlates of human nerve regeneration: ADCYAP1/PACAP enhance nerve outgrowth. Brain, 2020;7: 2009-2026.
- Zaccaria S, Di Perna P, Giurato L, P, et al. Diabetic polyneuropathy and physical activity in type 1 diabetes mellitus: a cross-sectional study. J Clin Med, 2023;12:6597.
- Kristensen F, Sanchez-Lastra M, et al. Leisure-time physical activity and risk of microvascular complications in individuals with type 2 diabetes: a U.K. Biobank study. Diabetes Care, 2023;46:1816-24.
- Streckmann F, Balke M, Cavaletti G, et al. Exercise and neuropathy: systematic review with meta-analysis. Sports Med, 2022 May;525:1043-65.
- Kanaley J, Colberg S, Corcoran M, et al. Exercise/physical activity in individuals with type 2 diabetes: a consensus statement from the American College of Sports Medicine. Med Sci Sports Exerc, 2022;1:353-68.
- Amanat S, Ghahri S, Dianatinasab A, et al. Exercise and type 2 diabetes. Adv Exp Med Biol, 2020;1228:91-105.
- Jenkins D, Jenks A. Exercise and diabetes: a narrative review. J Foot Ankle Surg, 2017;56:968-74.
- Smith A, Crippa A, Woodcock J, Brage S. Physical activity and incident type 2 diabetes mellitus: a systematic review and dose-response meta-analysis of prospective cohort studies. Diabetologia, 2016;59:2527-45.
- Naylor L, Davis E, Kalic R, et al. Exercise training improves vascular function in adolescents with type 2 diabetes. Physiol Rep, 2016;4:e12713.
- Akhtar S. Diabetes-induced peripheral neuropathy: Is prescribing physical exercise the answer? Biomol Biomed, 2024 Jan 11 (e-pub).
- Nuñez de Arenas-Arroyo S, Cavero-Redondo I, et al. Effects of exercise interventions to reduce chemotherapy- induced peripheral neuropathy severity: a meta-analysis. Scand J Med Sci Sports, 2023;00:1-14.
- McCrary, J. Matt, et al. Exercise-based rehabilitation for cancer survivors with chemotherapy-induced peripheral neuropathy. Support Care Cancer, 2019;27:3849-3857.
- Holmes C, Hastings M. The application of exercise training for diabetic peripheral neuropathy. J Clin Med, 2021 Oct 28;10(21):5042.
- Hammond E, Pitz M, Steinfeld K, et al. An exploratory randomized trial of physical therapy for the treatment of chemotherapy-induced peripheral neuropathy. Neurorehab Neural Repair, 2020;34:235-246.