New York's highest court of appeals has held that no-fault insurers cannot deny no-fault benefits where they unilaterally determine that a provider has committed misconduct based upon alleged fraudulent conduct. The Court held that this authority belongs solely to state regulators, specifically New York's Board of Regents, which oversees professional licensing and discipline. This follows a similar recent ruling in Florida reported in this publication.
Nomenclature and Classification of Lumbar Disc Pathology: Version 2.0
The Nomenclature and Classification of Lumbar Disc Pathology consensus, published in 2001 by the collaborative efforts of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology, has guided radiologists, clinicians and the public for more than a decade. The ASSR recently put together a task force to review and update the consensus document. Published in The Spine Journal, this updated document preserves the format and most of the terminology of the original document, with changes consistent with current concepts in radiological and clinical care. The modifications are intended to update and standardize the terminology and to provide greater clarity in the communication of findings between those who interpret images and those who make clinical decisions.
Let's look at the key modifications in the latest consensus, along with a brief list of some of the most common nomenclature that we may utilize to better communicate with our health care colleagues and patients. For more detailed information and an extended glossary, please refer to the complete document in The Spine Journal.
Glossary of Diagnostic Categories for the Lumbar Disc
The nomenclature / terminology focuses on the lumbar spine, as did the original consensus. As with the 2001 consensus, the assumption is that the same terminology can be extrapolated to the cervical and the thoracic spine.
The definitions describe the anatomy and pathology independent from etiology. The nomenclature is focused on describing the contour, content, integrity, organization and spatial relationships of the lumbar intervertebral disc. The nomenclature is intended for classification and reporting of imaging studies.
Diagnostic categories are based on pathology. These categories are as follows: normal, congenital / developmental variation, degeneration, trauma, infection / inflammation, neoplasia, and/or morphological variant of uncertain significance. Each diagnostic category can be subcategorized to various degrees of specificity in order to interpret the findings for a differential diagnosis.
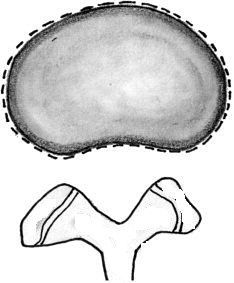
The Normal Disc
Normal means the disc is fully and normally developed, and free of any changes of disease, trauma, developmental issues or aging. Only the morphology is considered with this nomenclature, not the clinical context. The term normal for patient's age is not part of this nomenclature. The term only describes the morphology as it appears in the image. (Figure 1)
Annular Tear / Fissure
Annual tears / fissures include radial, transverse and concentric separations in the annulus indicating a loss in the integrity of the annulus. The term tear does not imply traumatic etiology. Annular tear and annular fissure are synonyms and do not imply a significant traumatic event. If a single traumatic event is clearly the source of loss of integrity of a formerly normal annulus, rupture of the annulus is the appropriate term.
Some tears have clinical relevance; others may be asymptomatic and inconsequential. The correlation of the characteristics of the tear with discography and contrast-enhanced MRI is still being debated and is beyond the scope of this classification system.
Herniated Disc
Herniated disc is a diagnostic term that describes disc material beyond the intervertebral disc space. Herniated disc, herniated nucleus pulposus, ruptured disc, prolapsed disc, protruded disc and bulging disc have all been used to describe displacement of disc material beyond the interspace. The meaning of these terms and the lack of definition of limits that should be placed on a general term has created a great deal of confusion in the clinical practice, and in the ability to even make meaningful comparisons in research studies.
In general, the term herniated disc means displacement of disc material beyond the interspace. The term herniated nucleus pulposus is inaccurate and should not be used because materials other than nucleus are common components of displaced disc material. Rupture implies the tearing apart and therefore suggests traumatic etiology, rather than displacement. Protrusion has been used by some in a nonspecific, general sense to signify any displacement; this term has a more specific meaning for which it is best reserved and should not be used for general disc displacement. (The use of protrusion will be discussed further under the heading of protruded discs.)
Prolapse has also been used an a general term as synonymous with the specific meaning of protrusion or to denote inferior migration of extruded disc material. It is confusing and best avoided.
Bulging Disc
Bulge and bulging disc mean a generalized extension of disc material beyond the edges of the apophyses of the vertebral endplates. The "bulging" involves more than 25 percent of the circumference of the disc and typically extends a relatively short distance – usually less than 3 mm beyond the edges of the apophyses. A disc bulge can be symmetrical throughout the circumference of the disc or it can be asymmetric. Bulge or bulging simply describes a morphological appearance and does not imply any specific etiology, prognosis or need for treatment.

By exclusion of the other terms and for reasons of simplicity and common usage, herniated disc is the best general term to denote displacement of disc material. This term is appropriate to denote the general diagnostic category. When the imaging data are sufficient to make the distinction, a herniated disc can be more specifically characterized as protruded or extruded. It should be noted that these distinctions are based on the shape of the displaced material and do not imply knowledge of the mechanism by which the changes occurred.
Protruded Disc
A disc is protruded if "the greatest distance between the edges of the disc material presenting outside the disc space is less than the distance between the edges of the base of that disc material extending outside the disc space. The base is defined as the width of the disc material at the outer margin of the disc space of origin, where disc material displaced beyond the disc space is continuous with the disc material within the disc space." (Figure 2)
The term protrusion is only appropriate in describing herniated disc material. Protrusions may be "focal" or "broad-based." The distinction between focal and broad-based is arbitrarily set at 25 percent of the circumference of the disc.
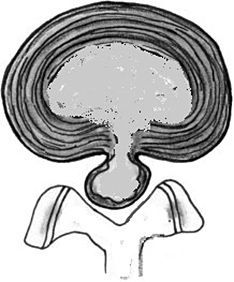
Extruded Disc
The term extruded means material is forced from one region to another through an aperture." In reference to a disc, an extrusion is present when "in at least one plane, any one distance between the edges of the disc material beyond the disc space is greater than the distance between the edges of the base measured in the same plane or when no continuity exists between the disc material beyond the disc space and that within the disc space." (Figure 3).
If the extruded disc material has no continuity with the disc of origin, it may be further characterized as "sequestrated." A sequestrated disc is a subtype of an extruded disc.
Note: Disc material can be displaced away from the disc of origin, regardless of continuity, and may be termed migrated, which is a useful term for interpretation because it is often impossible from the images to know if continuity exists.
Containment / Continuity
The terms contained and uncontained represent an attempt to distinguish whether or not the displaced disc material is held within an intact outer annulus. The technical limitations of currently available non-invasive imaging modalities (CT and MRI) usually preclude the distinction of contained vs. uncontained disc herniation. CT discography does not always allow one to distinguish whether the herniated components of a disc are contained, but only whether there is a communication between the disc space and the vertebral canal. Therefore, these terms are not reliable.
The terms capsule and subcapsular have been used to refer to containment by an unspecified combination of the annulus and posterior longitudinal ligament (PLL). These terms should not be used, as they are unclear and nonspecific.
In reference to the posterior longitudinal ligament, some have distinguished displaced disc material as "subligamentous," "extraligamentous," "transligamentous" or "perforated." When such distinctions are made, it is very difficult to tease out the difference between structures. Such refinements in the description of continuity, containment, and the relationship between ligaments and membranes may be of interest, but do not supersede the basic definition of disc herniation and the major subcategorization of extrusion and protrusion.
Details of the internal architecture of the intervertebral disc, in particular the annulus, are most often not visualized by even the best-quality MRI. The distinction of herniation is made by the observation of displacement of disc material beyond the edges of the ring apophysis of the vertebral endplate.
Author Notes
- Much of this nomenclature has been established by way of convention to lend precision to terminology, but this does not designate etiology, relation to symptoms or treatment indications.
- I wish to emphasize that this nomenclature and classification of lumbar disc pathology is for the purpose of describing the morphology of the disc as it is visualized in the various imaging modalities, i.e., CT and MRI. This terminology does not explain the etiology of the pathology it describes or the relationship to the symptoms presented by the patient.
Reference
- Fardon DF, et al. Lumbar disc nomenclature: version 2.0. Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J, 2014;14(11):2525-45.



