Some doctors thrive in a personality-based clinic and have a loyal following no matter what services or equipment they offer, but for most chiropractic offices who are trying to grow and expand, new equipment purchases help us stay relevant and continue to service our client base in the best, most up-to-date manner possible. So, regarding equipment purchasing: should you lease, get a bank loan, or pay cash?
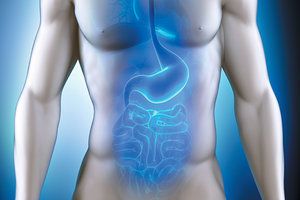
Understanding Hypothyroidism: The Gut Link
In part one of these articles we discovered the magnitude of hypothyroidism and the role it commonly plays in our patients. We also explored the necessity for a comprehensive workup and the optimal laboratory values for healthy thyroid function.
In part two we will discover the gut-thyroid-immune connection and the role it plays in the vast majority of hypothyroidism today. Currently more than 27 million Americans, mostly female, suffer with hypothyroidism and nearly half go undiagnosed.
The most surprising fact is that 90% of adult hypothyroidism is due to Hashimoto's thyroiditis. Hashimoto's is an autoimmune condition in which the cells of the thyroid are slowly destroyed by a misguided attack from the body's own immune system. In the beginning of Hashimoto's Thyroiditis, destruction of the thyroid cells causes a release of larger-than-normal amounts of T4 thyroid hormone, resulting in transient acute hyperthyroidism. With the destruction of the thyroid cells, eventually too few cells will remain to produce normal amounts of thyroid T4 hormone and the patient develops a hypothyroid state. Hashimoto's disorder is also the most common autoimmune disease in the US today affecting one in 10 of the US population. One of the most prominent reasons for this epidemic is the increase in toxic metals and chemicals in our environment causing altered immune function, also leading to chronic systemic infections and altered gut flora.
Gut-Immune-Thyroid Link
A healthy intestinal lining allows only beneficial substances and nutrients to be brought into the body for use. It therefore acts as a barrier system to keep unhealthy substances from passing through, including bacteria, yeasts, and their toxins, as well as undigested proteins and fats. About 70% of the total immune tissue of the body resides in the G.I. tract. This portion of the immune system is collectively known as gut-associated lymphoid tissue or GALT, a vital part of the intestinal barrier. GALT is made up of several types of lymphoid tissues, which contain immune cells such as T. and B. lymphocytes.
These lymphocytes are the attack dogs at the gates ready to strike and produce antibodies against any foreign invaders. This intestinal barrier system is vital because the gut is actually outside the body and traveling through it are multiple foreign substances and microbes that can damage the body.
Within a healthy digestive tract there should be over one hundred trillion beneficial bacteria and research is showing that an imbalance in your gut bacteria, called dysbiosis, is a contributing factor to many chronic as well as degenerative diseases, partly by causing an imbalance in your immune system function. This gastrointestinal dysbiosis is best understood as an over abundance of non-acute non-infectious GI microorganisms and/or a lack of beneficial bacteria, adversely affecting the human host.
As a result of a poor diet and environmental exposures including many different medications, especially antibiotics, the health of the gut bacteria can become compromised. This can damage the protective intestinal barrier of the gut. When the intestinal barrier becomes damaged and inflamed it becomes more permeable, often times referred to as "leaky gut syndrome." With this syndrome large foreign protein molecules can activate the GALT and escape the gut to enter the bloodstream leading to systemic wide problems. These undigested protein molecules that ‘leak' into the bloodstream can activate food allergy responses.
This launch of the immune system through food antigen activation plays a major role in autoimmune diseases including Hashimoto's. Gluten has now been shown to be a primary factor in the activation of Hashimoto's disease. It is advisable that all patients who have elevated thyroid antibodies be put on a diet completely free of gluten or the destruction of their thyroid will continue unabated.
Dysbiosis and subsequent increased intestinal permeability also allow the endotoxins or LPS from gram-negative bacteria in the gut to enter the bloodstream. These foreign proteins and endotoxins from unwanted gut bacteria cause local G.I. immune system activation and systemic inflammation. Recent studies have shown that this LPS immune activation plays a major role the development of autoimmune diseases and especially that of Hashimoto's.
As explained in part one, the inactive T4 release by the thyroid must be converted into the bioactive T-3. A little known role for healthy gut bacteria is to assist in the conversion of T4 into T-3. Nearly 20% of the T4 released by the thyroid is converted to forms of T3 in the G.I. tract. The conversion to active T-3 in the G.I. is accomplished by the enzyme sulfatase. Intestinal sulfatase is produced by healthy gut bacteria. Dysbiosis has been shown to significantly reduce the conversion to active T-3. Also dysbiosis induced inflammation of the gut also reduces the level of T-3 by raising cortisol which increases the conversion of T4 into reverse T-3.
Treating the Gut-Immune-Thyroid Link
The beginning point for this therapy is to address the underlying dysbiosis resulting in immune system activation. There are numerous factors in our modern lifestyle that can lead to this dysbiosis and increased intestinal permeability: overuse of antibiotics, poor diet, decreased digestive enzymes and maldigestion. If these factors can be eliminated or at least reduced, natural treatments aimed at dysbiosis will be more successful. High fiber diets with no simple carbohydrates have been shown to improve the quality and quantity of beneficial intestinal bacteria. Sugars and simple carbohydrates have been shown to feed the growth of unwelcome bacteria and yeast.
There are also specific antimicrobial herbs that can be used to directly kill or strongly inhibit unwanted intestinal microbes, such as Berberine sulfate. Herbs for dysbiosis are frequently continued for one to three months, and must be administered with very concentrated probiotics, taken three hours away from the antimicrobial herbs. Other herbs have been shown to have a strong influence on thyroid health and function.
Herbs Shown To Improve Hypothyroidism
Coleus forskohlii is an Ayurvedic herb that has been shown to actually increase thyroid gland hormone production and secretion into the bloodstream. Researchers have found that Coleus forskohlii also stimulates fat metabolism. Research has additionally found specific botanicals that help counteract hypothyroidism caused by the under conversion of T4 to T3 as discussed in part one of this article. Guggulsterones found in the Ayurvedic herb Guggul were found to help the body to convert T4 into T3, thereby increasing T3 levels.
Guggul extract guggulsterones also activates lipolytic enzymes increasing fat metabolism. Guggulsterones have been found to naturally regulate a gene receptor called farnesoid X receptor (FSX), which specifically turns on and off fat burning in the liver. Ashwagandha, another Ayurvedic herb used for thousands of years to boost stress tolerance and rejuvenate the body has been shown to help reduce the amount of damaging cortisol released in response to chronic stress. An elevation of cortisol has been shown to play a major role in hypothyroidism by causing the conversion of the T4 into the inactive reverse T-3. Ashwagandha is also a known promoter of T4 to T3 conversion, in part by improving overall liver function. Recently it has been shown that supplementation of a combination of resveratrol and Curcumin extracts have had a beneficial effect on slowing the destruction of the thyroid in Hashimoto's thyroiditis.
References
- Mori K, Nakagawa Y, Ozaki H, Does the gut microbiota trigger Hashimoto's thyroiditis?
- Discov Med. 2012 Nov; 14(78):321-6.



