It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
The Internally Rotating Hip
What happens when the hip tends toward internal rotation? This muscular imbalance can create pain in the anterior hip or groin, especially during flexion. This condition can also create posterior hip pain, masquerade as a vague sciatica, and/or contribute to chronic SI dysfunction and medial knee pain, ankle, or foot pain.
I wrote about Sahrmann's1 concept of the anterior femoral glide back in January.2 The medial rotation version of anterior femoral glide is the focus of the current article. In Sahrmann's view, there are two basic patterns of hip joint dysfunction. In both, the hip is usually stuck forward - the anterior femoral glide component. The pattern we are concerned with here involves too much internal rotation. This is more common in females, and correlates with pronation in the foot with medial knee pain, genu valgum and increased Q angles. The other pattern involves excessive external rotation and a lack of internal rotation in the hip joint, as I have written about previously.3
I experienced an epiphany while writing this article. I realized that for far too long, I missed this condition frequently in my patients. I just didn't "get it." My study group colleagues, and Shirley Sahrmann, describe the internally rotating hip as more common than the hip stuck in external rotation, but I was only rarely seeing it.
So, why was I missing this? Two reasons: First, I personally have a symptomatic externally rotated hip, so that experience tends to affect my "filters." Second, I am a chiropractor; I have a hard time with a condition that doesn't need an adjustment. If all you have is a hammer, everything looks like a nail. Even though I write about the importance of soft tissue and rehab, a condition that needs only soft tissue and rehab can escape my view. I've gotten over this blindness in the shoulder, in the elbow and the Achilles, all places where tendonosis responds so well to cross-frictional massage, but the internally rotated hip escaped me for a long time.
The internally rotated hip is primarily a muscular imbalance. The hip may lack external rotation, but not necessarily. The hip may have a hard end feel in either internal or external rotation, and the hip may be jammed forward in an anterior femoral glide. You cannot find this condition via palpation of any joint dysfunction. If it's strictly a muscular imbalance, you just need to release the tight soft tissues, and retrain and activate the inhibited muscles.
Diagnostic Considerations
The only way I know of to identify this condition is through a weight-bearing functional test. Here are the two variations I use. The patient is standing, and you ask them to do a lunge; to step forward with the front knee bent. You observe the forward knee, watching to see if it momentarily medially deviates. If the patient is stable on the forward knee as they do this, they have passed the test. If they are unstable on the front knee, with wobbling in the knee, especially in a medial direction, they probably have an internally rotated hip. You could also instruct them to step forward and up with one leg onto a small stool, and observe for the same medial deviation.
Other indicators include tests that identify the muscular imbalances more directly. Are the tensor fascia latae (TFL) and rectus femoris tight and short? This can be evaluated through the modified Thomas test and palpation. Are the gluteus medius and hip external rotators (piriformis, obturators, gemelli, and quadratus femoris) weak? The weight-bearing lunge test described above is directly aimed at identifying this weakness in a functional manner.

You can muscle test the deep lateral rotators. Have the patient sitting with their legs dangling. Then have them rotate inward with their foot against your resistance. Pushing the foot inward externally rotates the hip. Can the patient do this, especially at the end range? A muscle that has a chronic stress strain will be weak at end range. The clam shell exercise/test can be useful to identify this weakness as well, especially if you keep the patient's pelvis in neutral and don't let them rotate their pelvis backward as they lift their bent knee.
The Anterior Femoral Glide Component
The second component that usually accompanies the internally rotating hip involves an abnormal pattern of hip flexion. I discussed this in my anterior femoral glide article earlier this year. As the hip flexes, the proximal hip should drop backward, allowing freedom of hip flexion. This doesn't happen when the TFL and rectus femoris are too tight.
Hypertonic hamstrings can also contribute to this pattern. As you passively flex the hip, the patient will complain of groin pain. The patient will typically be tender to palpation over the femoral head.
You can easily determine whether an inferior-posterior glide will improve the hip flexion. As the patient flexes their upper leg, push the superior part of the femur inferior. (This would be a posterior pressure if the leg were straight.) If part of the problem is an anterior femoral glide, this pressure will ease the pain of hip flexion.
This can be useful as an assessment tool, as an in-office maneuver and as a home exercise. It may lend itself to anterior to posterior mobilization, and teaching the patient to mobilize the hip anterior to posterior during flexion.
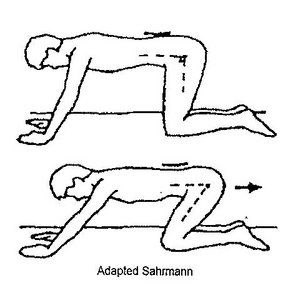
The two images above show two variations of exercise specifically to help this proximal hip glide. One uses a strap as the patient flexes. [Figure 1] This exercise can be done with the patient just holding the flexed position, as a long (2-minute) stretch, as shown in the picture. It can also be done as a self-mobilization with movement, having the patient further flex and then release the hip, with the strap as a fulcrum to guide the proximal hip inferior-posterior. The second exercise, a variant of child's pose from yoga, puts the body in a position to glide the proximal femur posteriorly. [Figure 2] To perform the exercise, the patient goes from a 90 degree position back to 120 degrees.
Soft-Tissue Treatment and Rehabilitation
Releasing the tissues of the obturator foramen seems to be very helpful for hips that are rotating internally. Despite the fact that in this model, these muscles are seen as weak, manual therapy with movement clearly seems to help. This is one of those sensitive areas most DCs don't touch. I suggest you observe a few cautions if you decide to examine and treat here. One, tell the patient what you are doing and why before you begin. Two, keep your hands on the lateral side of the pubic and ischial ramus. Never go medial to the bony structures.
The obturator muscles, both the internus and the externus, are involved. I contact the obturator foramen with my thumb or index finger. Remember to be gentle, especially in your first touch, as this is a sensitive area. The patient is supine in a hook-lying position. They can relax their bent leg outward as you support this area with your thigh. In this position, they are relaxed and the pelvis is open enough to easily get to the obturator.
I start with a contact on the lateral portion of the pubic symphysis, follow the pubic ramus slightly lateral, and then drop inferior toward the obturator foramen. The contact presses superior and medial. You'll feel as though your finger or thumb is pressing into a trampoline. Look at a 3-D model and see how the obturator foramen faces inferior and lateral. I will vary the exact location of my contact to find the most tender area in the foramen. It could be central, more medial or more superior-medial.
I maintain this contact and then have the patient actively push their knee outward against my resistance, creating external rotation in the hip. It's not just isometric; have them move a few inches and you'll feel a muscular activation under your contact hand. It's the obturator muscles that are firing. If this area is significant, you may get better range of motion after performing this procedure.
The other critical muscle to inhibit or downtrain is the TFL. Stretching the TFL, doing cross-frictional massage or Graston Technique to the TFL, and using inhibitory taping can all be helpful. The TFL belly is short, but it has a long-lever arm and is a significant internal rotator, especially when the posterior muscles are inhibited.
Here are the keys to an effective stretch of the hip flexors with a bias toward the TFL. The leg you are stretching should be externally rotated; this helps focus on the TFL. It is critical that the patient maintain a posterior pelvic tilt, activating tucking the pelvis underneath them. If they don't, they can sublux their iliosacral joint with this stretch.
One version of the stretch is done standing, if the patient has enough strength, flexibility and stability. Have them stand on the non-involved side with the knee slightly bent, and fully bend the involved leg at the knee. Grab the ankle or foot with the opposite arm, thus externally rotating the involved leg. Activate the abs and glutes to strongly initiate a posterior pelvic tilt. Actively push the involved knee toward the ground inferiorly. The patient should feel a strong stretch in the anterior thigh. There are plenty of variations of this stretch, done prone or side-lying. Use of a strap may help.
The gluteus medius and the small hip external rotators (piriformis, gemelli, etc.) are probably inhibited. You want to retrain them. It may be helpful to do a deep form of soft tissue, such as Graston, or manual deep pressure, as the patient externally rotates and abducts. Pay particular attention to the insertions of the deep lateral rotators into the back of the greater trochanter. This can be best assessed and treated side-lying.
It is a challenge to properly train the patient in home exercises for the hip abductors (gluteus medius). The patient is likely to substitute with the already overactive TFL. In the clam shell and side-lying leg-lift positions, if the patient rotates the pelvis posterior in the transverse plane, they are cheating by lining up the TFL or rectus femoris to help them. Pay close attention to positioning and make sure the gluteus medius is firing, not the TFL.
The other key soft-tissue issue is recognizing that "piriformis" pain - pain or tenderness behind the greater trochanter - does not automatically mean that the piriformis and the other lateral rotators are tight. When the hip tends to internally rotate, theses muscles tend to get stretched out and weak. The pain can be a stretch-strain pattern. This indicates a muscle that is stretched into length and irritated.
Don't stretch it; strengthen it. The posterior hip will feel tight to the patient, but they should not stretch it, because that just reinforces the pattern. That doesn't mean the piriformis doesn't have trigger points. Weak muscles also benefit from soft-tissue work.
We see the psoas as primarily a stabilizer of the hip and lumbar spine. In the hip, its primary function is to pull superior on the femur, sucking the hip up into the joint. It will often need retraining. (I also addressed this in the anterior femoral glide article.)
Finally, don't forget the rest of the core. These folks may need increased core endurance and motor control. Other significant muscles include the hamstrings and the adductors.
The typical medical diagnosis for most posterior hip pain is trochanteric bursitis. I am skeptical about whether the bursa is actually inflamed. In my opinion, the bursa and/or other soft tissues are probably irritated due to the chronic stress strain of the external rotators as they insert into the greater trochanter. I also think the answer is normalizing the biomechanics, rather than starting with a cortisone injection. If deep-tissue work and rehab help this pain pattern, it is probably not a true bursitis, but an insertional tendonopathy or periosteal irritation, secondary to the stretch-strain.
The diagnosis of piriformis syndrome is a strange one to me. The piriformis is clearly a player here, but it is important to understand why. I think "piriformis syndrome" is secondary to hip and SI dysfunction, and that the piriformis is just one player in this symphony.
References
- Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis: Mosby, 2002.
- Heller M. "Anterior Femoral Glide Syndrome." Dynamic Chiropractic, Jan. 1, 2009.
- Heller M. "The Hip Joint: Myofascial and Joint Patterns." Dynamic Chiropractic, May 7, 2007.



