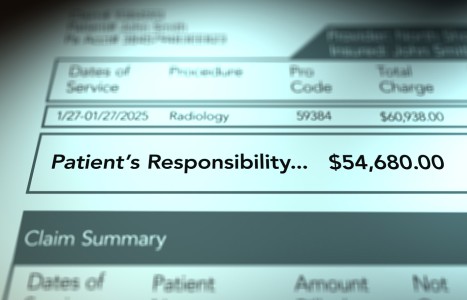
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
ACC Focuses on Informed Consent
The Association of Chiropractic Colleges (ACC), representing all accredited U.S. chiropractic educational programs and three international programs, has completed an informed consent guideline for its member institutions. The ACC states that while the guideline is not intended to have the force of law, chiropractic educational programs are encouraged to adopt and teach the recommended protocols to maximize the patient experience.
"The document and study is a result of over a year of work led by a committee chaired by Clay McDonald, DC, JD, and his peers and supported by a vote of the ACC Board," said ACC President Carl Cleveland III, DC. "It is appropriate and timely to help clarify this important professional topic."
According to the ACC, "The Informed Consent Doctrine stems from the concept that patients have the right to control their body and what happens to it. Therefore, to be in control, they have the right to be informed about the proposed care and the risks associated with it. The [ACC] believes when patients receive appropriate information (informed consent) before undergoing chiropractic care, it will assist in eliminating misunderstandings." The ACC guideline specifies when consent should be contained, who can give informed consent, what information should be disclosed to the patient, and how consent should be documented. Excerpts from the guideline are reprinted as follows:
When to Obtain Consent
"[F]ailure to obtain the informed consent of a patient before performing a particular diagnostic or clinical procedure impairs the right of that patient to decide for him/herself what, if any, care he/she wishes to undergo. As new complaints arise requiring additional evaluation procedures or different care procedures additional informed consent should be acquired from the patient.
"The Doctor providing a particular diagnostic or clinical procedure (not a delegated representative) should disclose and discuss with the patient the elements of informed consent in layman's terms. In turn, the patient should have an opportunity to ask questions to elicit a better understanding of the particular diagnostic or clinical procedure, so he/she can make an informed decision to accept or to refuse a particular course of health intervention."
Who Can Give Consent?
"It is reasonable to assume that an adult patient is capable of giving consent for diagnosis and care, unless there are indications or other known factors that the patient is not mentally competent to understand what is proposed and the potential benefits and risks involved. If the Doctor reasonably believes that an adult patient does not adequately understand what is proposed and the related potential benefits and risks, the Doctor should decline to provide care and should inquire as to whether the patient has a legal guardian or health care proxy with the legal authority to make the necessary decisions.
"When the patient is a minor, the Doctor should obtain the necessary informed consent from the parent or legal guardian of the patient, as a general rule the consent of only one parent is necessary to permit care. There may be certain limited circumstances under which a minor child is considered emancipated and thus can legally and effectively consent for himself or herself. When in doubt, seek legal advice from the member institutions general counsel to confirm that emancipation is in place and thus consent of an adult is not required."
What Information Should Be Disclosed?
"The Doctor should disclose to the patient all significant clinical information that the Doctor possesses, which would be material to the decision by that patient whether or not to undergo the proposed procedure. For the consent to be legally effective, the patient must receive sufficient information concerning: the proposed procedure; the potential benefits and risks of the procedure; common alternatives to that procedure, including refusing care and the associated risks. Without this disclosure, an informed decision cannot be made."
Documentation of Consent
"The [ACC] recommends that the Doctor engage in a thorough, verbal discussion with the patient, thus enabling the Doctor to be in a position to verify that he/she took the time to explain the material risks inherent in the recommended procedures and that the patient consented. Beyond this, the [ACC] recommends that the patient execute some document acknowledging that: (a) he/she has been part of an informed consent process; (b) that the material risks have been disclosed to the patient, including a description of those material risks; and (c) that the patient, after assessment, has agreed ("consented") to the procedures understanding any material risks which are inherent to that procedure.
"It is the [ACC's] belief that the profession and the public interest are better served by an occasional patient refusing to execute an informed consent acknowledgment form as opposed to having licensed Doctors exposed to claims of informed consent violations when, in fact, informed consent was secured but not irrefutably documented and verified. It is the recommendation of the Association of Chiropractic College's to document the patient's consent to both the diagnostic procedures which the practitioner proposes to use, as well as to document the patient's consent to the "patient care plan" which lists the patient's diagnosis and identifies the particular procedures and/or modalities to be used."
In the guideline's conclusion, the ACC recommends the following steps be taken to implement appropriate informed consent in all member institutions: (1) Ongoing training for all current faculty and faculty clinicians. This will include a process by which new faculty will be trained in the interim, addressing guideline implementation at all member institutions. (2) Implementation of a program throughout member institutions to ensure students adequately learn the specifics of informed consent, and to ensure compliance and educational instruction are achieved at every level of the educational encounter. (3) Report of findings to patients at all member institutions that includes all elements of informed consent, consistent with best practices. (4) Review and updating of all required elements of ACC guideline as appropriate.
While the ACC informed consent guideline is intended first and foremost for the association's member educational institutions, including faculty and students, practicing doctors of chiropractic will surely find it valuable for future interactions with patients. To learn more about the guideline, contact the ACC via e-mail (info@chirocolleges.org).