Some doctors thrive in a personality-based clinic and have a loyal following no matter what services or equipment they offer, but for most chiropractic offices who are trying to grow and expand, new equipment purchases help us stay relevant and continue to service our client base in the best, most up-to-date manner possible. So, regarding equipment purchasing: should you lease, get a bank loan, or pay cash?
Calcium Score: What Is It?
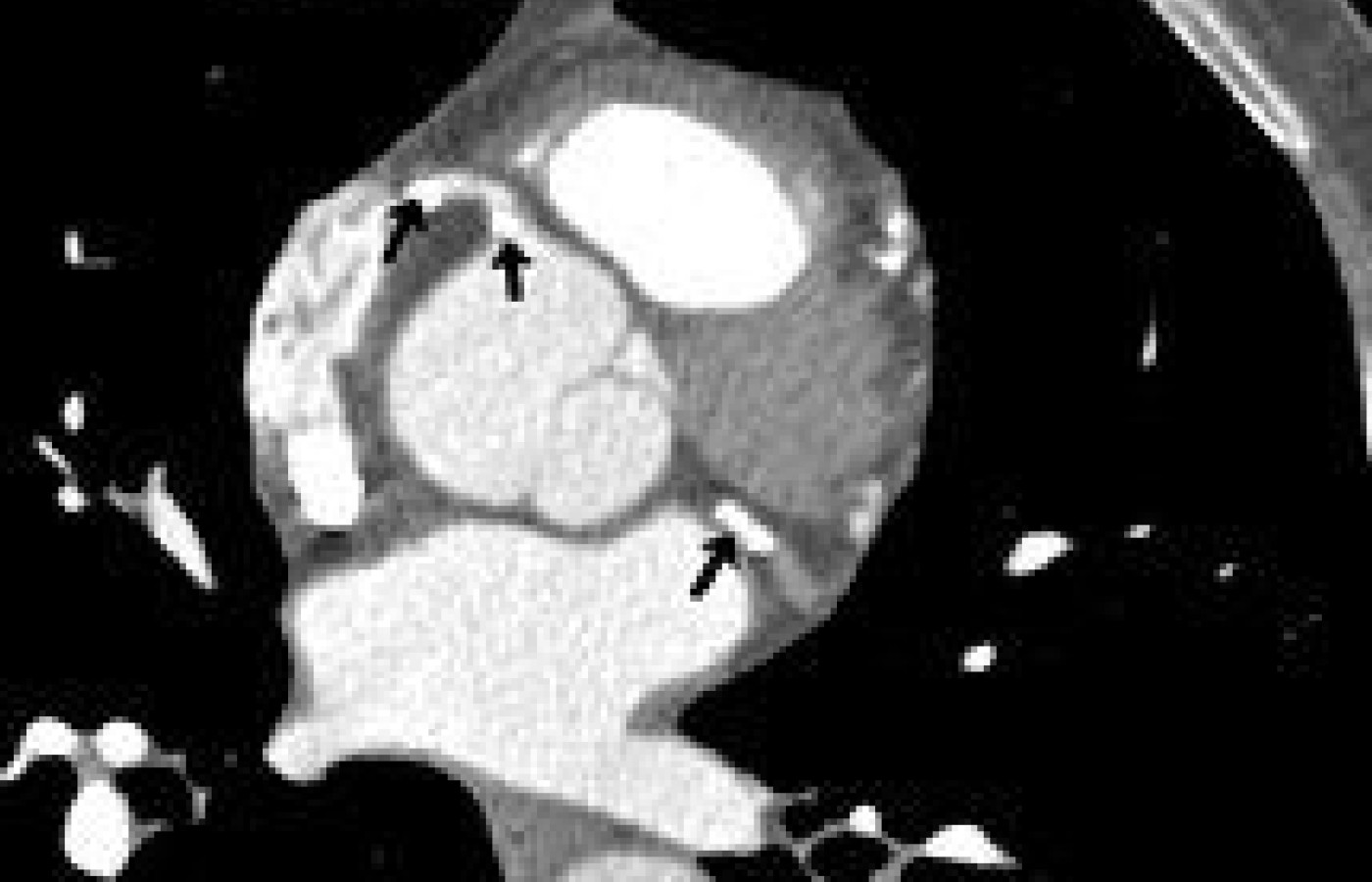
Coronary artery disease (CAD) is the number-one cause of death in the Western world. Therefore, being able to detect this disease, particularly early on, before invasive measures are necessary, is extremely important. We have effective treatments for this major health problem. This topic has recently been most eloquently reviewed by one of our very own, Dr. James Meschino.1 A discussion of the etiology of coronary artery disease is beyond the scope of this article. The topic for this article is simply the use of cardiac CT and the calcium score for detecting CAD.

A total calcium score is derived by summing individual lesion scores from each of four anatomic sites (left main, left anterior descending, circumflex, and right coronary arteries). This calculation becomes the calcium score. There is a direct correlation between the extent of calcium in the coronary arteries and the risk of a future cardiac event (heart attack). For example, a calcium score of more than 400 is considered severe, and it would be necessary to take steps to prevent further advancement of atherosclerosis and plaque formation. The higher the calcium score, the more likely there is severe stenosis. On the other hand, a calcium score of 0 does not rule out the existence of soft plaques, but statistically rules out significant coronary artery disease. Though the calcium score does not allow us to evaluate the incidence of soft plaques, it does alert us to the presence and extent of CAD. The higher the calcium score, the more likely soft plaques are present. (Remember that the rupture of a soft plaque is the most common cause of acute coronary syndrome.)2
| Calcium Score | Presence of Plaque |
| 0 | No evidence of plaque |
| 1-10 | Minimal evidence of plaque |
| 11-100 | Mild evidence of plaque |
| 101-400 | Moderate evidence of plaque |
| Over 400 | Extensive evidence of plaque |
In the past, guidelines have regulated that all adults undergo coronary heart disease (CHD) risk assessment using the Framingham risk score (FRS) as the standard. (See http://hp2010.nhlbihin.net/atpiii/calculator.asp?usertype=prof.) Now, there is compelling evidence that this risk assessment can be improved with the addition of coronary artery calcium scoring (CACS).3 We have the tools to detect CAD before individuals develop symptoms, and can intercede with proper management to prevent progression of the disease. We can even possibly reverse the process.
Unfortunately, as with many diagnostic tools, there is a cost factor. To date, many insurers have not reimbursed for this test, especially for younger individuals. Hopefully, this will change in the near future, as mounting data indicate it is cheaper to prevent coronary artery disease than it is to treat it.
References
- Meschino J. "Helping Patients Achieve a Cholesterol Level Below 150 mg/dL." Dynamic Chiropractic, April 9, 2007. www.chiroweb.com/archives/25/08/30.html.
- Schoepf UJ, Becher CR, Ohnesorge BM, Yucel EK. CT of coronary artery disease. Radiology, July 2004;232(1):18-37.
- Greeland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA, 2004;291:210-5.