It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Differentiating Sources of Low Back Pain: Palpation Tools
Mechanical back pain, or nonspecific back pain, are terms for pain coming from various sources, commonly described as including sensory receptors from joints, ligaments, tendons, and muscles, as well as from the annulus of the disc. As chiropractors, we attempt to be more accurate in differentiating the sources of back pain.
This article focuses on palpation findings in the lumbar spine. I recognize that there are many other diagnostic tools that help us with this differentiation, including imaging studies, ROM, pain provocation and pain-relieving positions.
Tenderness over a specific structure can help us isolate the pain-generating tissue. The best clinician does not automatically treat the pain generator. If the pain generator is a hypermobile joint, accompanying hypomobile joints may need adjusting, and the stabilizing muscles that allow the hypermobility may need retraining. Pain is a liar; we need to search for the cause. The pain generator concept is extremely useful as an entry point, as an exam finding to tell us what you are trying to change via your treatment, and as a recheck at the end of the session.
I use my hands to detect more than tenderness. I check for mobility; I "listen" for what tissues pull me in, and I feel for soft-tissue changes. Of all of the information I can get from palpation, the most reliable, the most studied as accurate in interexaminer studies, is tenderness.1 Despite this, tenderness seems to be underutilized as a diagnostic tool in many chiropractic techniques.
Let's discuss using palpation to assess for three categories of low back pain. The first is lumbar facet joint pain. The second is sacroiliac joint pain. The third is discogenic or dural pain elicited through midline tenderness. I could add a fourth category of muscular/tendonous origin of mechanical pain, but there are musculotendonous aspects of all three of the other categories. I am leaving out nerve root pain (sciatica), stenosis, hip joint pain and degenerative joint disease.
These palpation tests are done with substantial pressure, measured in pounds, rather than ounces. You are attempting to elicit tenderness, so keep your patient alert, and ask, "Does this spot hurt?"
How do I assess for lumbar facet pain? The specific palpation methods I describe here are a variation on the methods used in "muscle energy," a low-force osteopathic technique. The pain generator could be the facet joint itself, or dysfunction of the deep lumbar muscles. The tenderness will be found paraspinally, usually a sharper tenderness over one or two levels, usually unilateral. These three tests can evaluate simultaneously for tenderness and for lack of motion. I test with the patient in a sitting position, so that I can move him or her into both lumbar flexion and extension; rather than prone, where motion is much more limited.
First, with the patient sitting, have him or her slump into lumbar flexion, to test whether the facets can flex or open. Test the facet joint with pressure from the posterior and inferior, pushing anterior and superior, to challenge the closed facet, attempting to open it. I have described the basic correction for this joint pattern previously.2 This article addresses the thoracic spine, but similar techniques work well in the lower lumbar.
The second and third tests evaluate whether the facet can extend. They are also done while the patient is sitting.

For the second test, have the patient in a neutral spine position, with a slight lordosis, and push the facet anterior and slightly inferior, stressing the joint into extension. You may want to add a right lateral bending to this component. If this is tender and stiff, the involved facet lacks the ability to extend at that level.
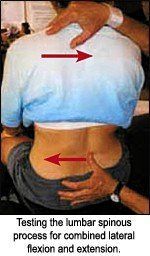
The third test is for the same motion, but uses the spinous process as the lever. Test the spinous processes of the lower lumbars by pushing from the side, while slightly extending the whole lumbar spine. If you are pressing from right to left on L4, for example, you could use your left thumb on the L4 spinous. The patient should have his or her arms crossed, while your right arm controls the whole body of the patient by holding the left shoulder and whole upper body, moving the entire trunk into right lateral bending with slight extension. This tests L4, looking for a lack of extension and right lateral bending. I find the spinous process the most accurate tenderness indicator when there is a lack of extension. Corrective techniques for this spinal lesion are described in a previous article.3

The sacroiliac ligaments were well-described in my last article,4 so I will be brief here. When any of the ligaments directly over the joint is tender, or when the sacrotuberous ligaments are tender to deep palpation, you almost certainly have an SI involvement. One key tender spot is at the S3 or S4 level, on the sacral side of the involved SI joint. Tenderness over the iliolumbar ligament seems to occur in both SI and lumbar facet problems. The gluteus maximus origins from the sacrum are also usually tender in an SI problem.
Midline tenderness is one of my favorite topics, and I think this phenomenon is missed far too often. It can be missed because the doctor is not checking for it, or because the interspinous space is not being accurately assessed. I have watched examiners just spring the spinous in a posterior to anterior direction. This frequently misses the midline tenderness finding, which can be assessed with the patient either sitting or prone.
For a sitting test, have the patient slumped into lumbar flexion. Use your thumb in the interspinous spaces. Press posterior to anterior, with a slight superior pressure. You can also test this prone, whereby you take advantage of gravity. Put a pillow under the patient's tummy, or use SOT blocks under the ASIS, to take the patient out of lordosis. Use your thumb to press posterior to anterior, and press superior, at the interspinous spaces. When a particular disc level is irritated, you will usually elicit a sharp pain with your pressure. If the pain lasts several minutes from this pressure, it's a strong indicator of an inflamed disc. Begin with moderate pressure, as this space can be exquisitely sensitive. Sometimes, you will need a more substantial pressure. I have previously written about midline tenderness as an indicator of discogenic axial pain.5
I find that midline tenderness indicates either discogenic pain or dural pain. There is limited evidence to support this. There are two studies6,7 that used a modified Oral B toothbrush, in which tenderness to deep vibration correlated with discogram findings. Axial discogenic pain can be such a puzzle. Patients with equivocal or mildly positive MRIs may or may not have pain from their disc.

Irritation of the dura is an even less-well-researched diagnostic impression. It depends on even more subtle palpation findings of a restriction of dural glide. This has been taught extensively in the cranial field, and is referenced in AK, SOT, and other chiropractic methods, but it is not really part of our dominant chiropractic paradigm. When I find a series of midline tender points, for example, L3-4, L4-5, and L5-S1, I strongly suspect dural irritation, a more global involvement of the dura. This can be secondary to a disc problem or to any restriction in the dura anywhere along the craniosacral axis.
Specific lumbar tenderness is relatively simple to find, once you know exactly where to look. You can improve the specificity of your diagnostic impression by knowing which joints are irritated and tender. You can use changes in these tender points as indicators of objective progress. The art of chiropractic demands accuracy for optimal results.
References
- Christensen HW, Vach W, Vach K, et al. Palpation of the upper thoracic spine: an observer reliability study. J Manipulative Physiol Ther June 2002;25(5):285-92. Erratum in: J Manipulative Physiol Ther Jul-Aug 2002;25(6):425.
- For spinal segments resisting flexion: Heller M. The upper thoracic spine and posterior ribs. Dynamic Chiropractic, Sept. 24, 2002: www.chiroweb.com/archives/20/20/07.html.
- For spinal segments resisting extension: Heller M. Subluxation and muscle patterns for the lower thoracics. Dynamic Chiropractic, Nov. 4, 2002: www.chiroweb.com/archives/20/23/10.html.
- Heller M. Sacroiliac revisited - the importance of ligamentous integrity. Dynamic Chiropractic, July 2, 2005: www.chiroweb.com/archives/23/14/10.html.
- Heller M. Discogenic pain - diagnosis and treatment. Dynamic Chiropractic, Sept. 1, 2003: www.chiroweb.com/archives/21/18/08.html. Also: Heller M. Correction of discogenic pain and midline tenderness: www.chiroweb.com/archives/21/21/09.html.
- Yrjama M, Tervonen 0, Kurunlahti M, Vanharanta H. Bony vibration stimulation test combined with magnetic resonance imaging. Can discography be replaced? Spine 1997;22(7):808-13.
- Vanharanta H, Ohnmeiss D, Aprill C. Vibration pain provocation can improve the specificity of MRI in the diagnosis of symptomatic lumbar disc rupture. Clin J Pain 1998;14:239-247.



