It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
DISH - What Is It? What Does It Mean When Detected?
Diffuse Idiopathic Skeletal Hyperostosis (DISH) is a relatively common degenerative condition seen in approximately 28% of cadavers at autopsy. It is more common in men than women and affects patients over the age of 55, but can begin as early at age 40.1
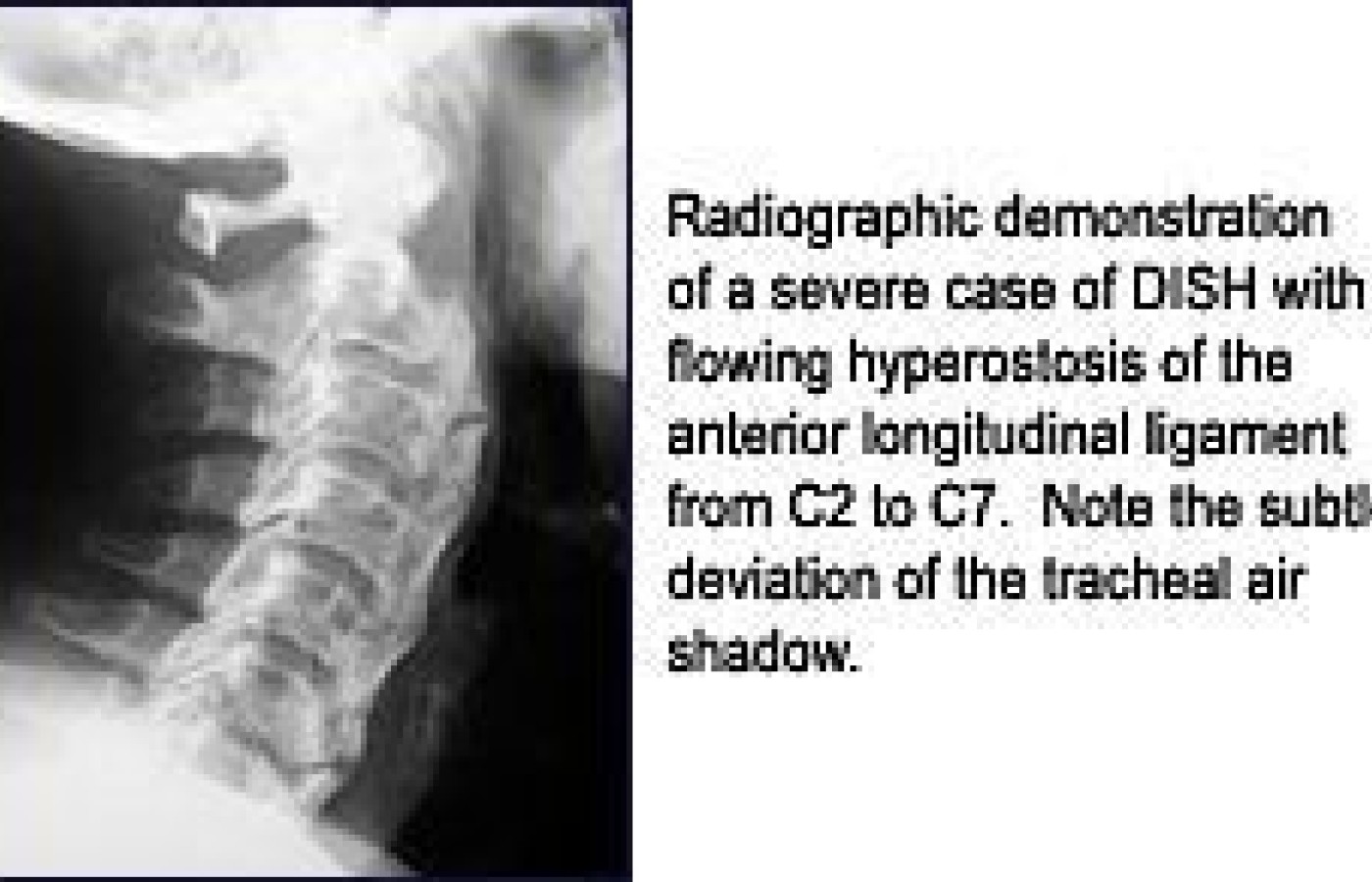
The etiology of DISH is unknown, and it typically manifests as calcification/ossification of ligaments, primarily the anterior longitudinal ligament (ALL) of the spine. Patients generally present with DISH as an incidental finding; however, difficulty swallowing and reduced range of motion may also be present. Typical radiographic findings include a flowing hyperostosis or dense calcification/ossification anterior to the vertebral bodies, and according to the diagnostic criteria, this flowing hyperostosis must span at least four continuous segments.
In addition, the diagnostic criteria must also include the absence of facet and sacroiliac joint involvement.1 This is especially important to remember because the purpose of the criteria is to assist in eliminating inflammatory conditions (such as psoriatic arthritis and ankylosing spondylitis) as possible diagnoses. These inflammatory conditions do affect the facet and sacroiliac joints, along with the presentation of paravertebral and vertebral calcification/ossifications (syndesmophytes), and can therefore be confused with DISH.
Once the diagnosis of DISH is made, there are commonly coexisting conditions or complications that must be investigated. Of particular importance to chiropractors, who will perform spinal adjustments, is to rule out calcification/ossification of the posterior longitudinal ligament (OPLL). This is seen in up to 50% of DISH patients and will narrow the spinal canal, typically in the upper cervical region.1 This can lead to neurologic compromise.

Other possible complications of DISH arise when exuberant calcification/ossification of the ALL leads to reduced range of motion; the possibility of fracturing through the calcified ligaments also exists. Consequently, caution should be exercised when adjusting these patients. Also, if the patient presents with dysphagia/difficulty swallowing associated with DISH, surgical resection may be necessary to eliminate the mass effect of the calcified/ossified ALL upon the esophagus. Along with the neuro-musculoskeletal manifestations of DISH, there is up to a 32% coincidence of DISH and diabetes mellitus.1 The thorough clinician should follow up a diagnosis of DISH with laboratory investigation of fasting blood glucose to rule out diabetes, if the patient has not already been diagnosed with or is being managed for that condition.2
References
- Resnick, D., Niwayama, G. Diagnosis of Bone and Joint Disorders, 3rd ed. Philadelphia: W.B. Saunders, 1995: pp.1463-1495.
- Fishbach, F. A Manual of Laboratory and Diagnostic Tests, 4th ed. Philadelphia: J. B. Lippincott, 1992: pp.296-298.
John M. Bassano, DC, DACBR
Associate Professor,
Dept. of Diagnostic Imaging
Los Angeles College of Chiropractic
Southern California University of Health Sciences