It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
What's All the Buzz About Spinal Stability? Part One: Biomechanics and Neurophysiology
The concepts of stability and instability are integral to modern musculoskeletal care. According to Panjabi, three subsystems work together to maintain spine stability:1 the central nervous subsystem (control), an osteoligamentous subsystem (passive), and a muscle subsystem (active). He says: "The neural subsystem receives information from the transducers, determines specific requirements for spinal stability, and causes the active subsystem to achieve the stability goal."
The spine or any joint becomes injured or irritated by end-range overload. This can involve either macrotrauma or repetitive micro-trauma. Motor control is a key component in injury prevention. Impaired motor control consists of failure to control a joint's "neutral range," usually by a dysfunction or incoordination of the agonist-antagonist muscle co-activation. The eminent researcher Professor Stuart McGill states, "Evidence from tissue-specific injury generally supports the notion of a neutral spine (neutral lordosis) when performing loading tasks to minimize the risk of low back injury."2
The spinal column, devoid of its musculature, has been found to buckle at a load of only 90 newtons (about 20 pounds) at L5.3,4 However, during routine activities, loads 20 times greater are encountered on a regular basis.(Load profiles of various activities are shown below.)
Spinal Load Profiles
- Without muscles, the spine buckles at 90N.20
- Routine activities of daily living involve ≈ 2000N.1
- According to McGill, recommended subacute exercise training < 3000N.22
- National Institute for Occupational Safety and Health (NIOSH) limit for repetitive tasks: 3300N.18
- NIOSH work demand limit: 6400N.23-25
- Competitive weight lifters manage loads in excess of 20,000N (4,480 lb).26
Panjabi says, "This large load-carrying capacity is achieved by the participation of well-coordinated muscles surrounding the spinal column."1
Surprisingly, the motor control system functions well when under load. Muscles stabilize joints by stiffening, like rigging on a ship:
According to Cholewicki and McGill,5 spine stability is greatly enhanced by co-contraction of antagonistic trunk muscles (e.g., abdominal and extensor muscles). Co-contractions increase spinal compressive load, as much as 12% to 18%, or 440N, but they increase spinal stability even more by 36% to 64%, or 2,925N.6 But when load is at a minimum, such as when the body is relaxed or a task is trivial, the motor control system is often "caught off guard" and injuries are precipitated.
Low back injury has been shown to result from repetitive motion at end range: According to McGill, it is usually a result of "a history of excessive loading which gradually, but progressively, reduces the tissue failure tolerance."2
Inappropriate muscle activation sequences during seemingly trivial tasks (only 60 newtons of force), such as bending over to pick up a pencil, can compromise spine stability and potentiate buckling of the passive ligamentous restraints.7 This motor control skill has also been shown to be compromised under challenging aerobic circumstances.8-10
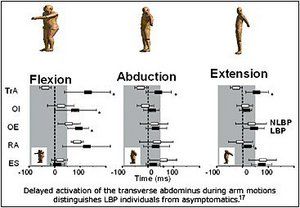
A persuasive body of literature from Australia has demonstrated how altered motor control is related to back pain. Hodges and Richardson reported that a slow speed of contraction of the transverse abdominus during arm or leg movements was well-correlated with LBP.11,12
O'Sullivan, et al., found that synergist substitution of the rectus abdominus for the agonist transverse abdominus during an abdominal "drawing-in" maneuver strongly correlated with chronic back pain, and that specific rehabilitation that improved this dysfunction was superior to a more general exercise approach.13
The multifidus in the low back has been shown to be atrophied in patients with acute low back pain.14 The acute patients' atrophy was unilateral to the side of pain and at the same segmental level as palpable joint dysfunction. Recovery from acute pain did not automatically result in restoration of the normal girth of the muscle. However, it has been demonstrated that segmental spinal stabilization exercises can prevent multifidus muscle atrophy in acute LBP subjects.15 Recent research has demonstrated that such exercises have a secondary preventive effect by reducing recurrences.16
Delayed activation of the transverse abdominus during arm motions distinguishes LBP individuals from asymptomatics.19
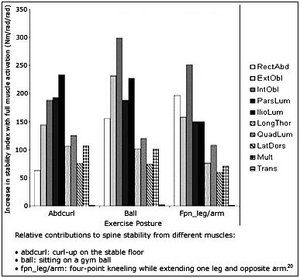
The Australian research clearly shows that motor control errors correlate with LBP, but it has been misintrepreted as proving that certain individual muscles have a unique role in producing stabililty.17 Recent studies have shown that all muscles function as stabilizers, depending on the task.18 Plus, the relative output varies throughout the movement so that discussion of the most important muscle is restricted to a transient instant in time.
Conclusion
Spinal instability potentiates joint disorders. Spine stability requires that the central nervous, joint, and muscle systems all work together. The joints are primarily passive, while the muscles are the active components that execute the commands of the nervous system. Part two of this series will discuss assessment and treatment approaches for identifying spine instability and promoting stability.
References
- Panjabi MM. The stabilizing system of the spine. Part 1. Function, dysfunction, adaptation, and enhancement. J Spinal Disorders 1992;5:383-389.
- McGill SM. Resource manual for Guidelines for Exercise Testing and Prescription, 3rd ed. Williams and Wilkins, 1998.
- Crisco JJ, Panjabi MM. Euler stability of the human ligamentous lumbar spine. Part 1: theory. Clinical Biomechanics 1992;7:19-26.
- Crisco JJ, Panjabi MM, Yamamoto I, Oxland TR. Euler stability of the human ligamentous lumbar spine. Part 2: Experimental. Clinical Biomechanics 1992;7:27-32.
- Cholewicki, J., and McGill, S.M. Mechanical stability of the in vivo lumbar spine: Implications for injury and chronic low back pain, Clin Biomech 1996;11(1):1-15.
- Granata KP, Marras WS. Cost-benefit of muscle cocontraction in protecting against spinal instability. Spine 2000;25:1398-1404.
- Adams, M.A., Dolan, P. Recent advances in lumbar spine mechanics and their clinical significance. Clin Biomech 1995;10:3-19.
- McGill SM, Sharratt MT, Seguin JP. Loads on the spinal tissues during simultaneous lifting and ventilatory challenge. Ergonomics 1995;38:1772-1792.
- Hodges, PW, McKenzie, DK, Heijnen, I and Gandevia, SC. Reduced contribution of the diaphragm to postural control in patients with severe chronic airflow limitation. In Procceedings of the Thoracic Society of Australia and New Zealand. Melbourne, Australia, 2000.
- OÕSullivan PB, Beales DJ, Beetham JA, Cripps J, Graf F, Lin I, Tucker B, Avery A. Altered motor control strategies in subjects with sacroiliac joint pain during the active straight-leg-raise test. Spine 2002;27:E1-E8.
- Hodges PW, Richardson CA. Delayed postural contraction of the transverse abdominus associated with movement of the lower limb in people with low back pain. J Spinal Disord 1998;11:46-56.
- Hodges PW, Richardson CA. Altered trunk muscle recruitment in people with low back pain with upper limb movements at different speeds. Arch Phys Med Rehabili 1999;80:1005-1012.
- OÕSullivan P, Twomey L, Allison G. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolysthesis. Spine 1997;24:2959-2967.
- Hides JA, Stokes MJ, Saide M, Jull Ga, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine 1994;19(2):165-172.
- Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automaticafter resolution of acute, first-episode of low back pain. Spine 1996;21(23): 2763-2769.
- Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine 2001;26:e243-e248.
- Hodges PW, Jull G in Rehabilitation of the Spine, 2nd edition. (ed. Liebenson C) Lippincott, Williams & Wilkins, sched. pub. 2005.
- McGill SM. Low back disorders. In: Evidence-Based Prevention and Rehabilitation. Human Kinetics Publishers, Champaign, Ill., 2002.
- McGill S, Grenier S, Bluhm M, Preuss R, Brown S, Russell C. Previous history of LBP with work loss is related to lingering deficits in biomechanical, physiological, personal, psychosocial and motor control characteristics. Ergonomics 2003;46:731-746.
- McGill S. Rehabilitation of the Spine, 2nd ed. (Liebenson C, editor). Lippincott, Williams & Wilkins, sched. pub. 2005.
- Crisco JJ, Panjabi MM. Postural biomechanical stability and gross muscular architecture in the spine. In: Winters JM, Woo SL-Y (eds.): Multiple Muscle Systems. Chapter 26, pp238-50. Springer-Verlag, New York, 1990.
- McGill SM. The biomechanics of low back injury: implications on current pratice in iIndustry and the clinic. J Biomechanics 1997;30(5):465-47.
- Gardner-Morse MG, Stokes IA. The effects of abdominal muscle coactivation on lumbar spine stability. Spine 1998;23:86-91.
- Gordon SJ. Mechanism of disc rupture - a preliminary report. Spine 1991;16:45.
- Stokes IAF, Garnder-Morse M, Henry SM, Badger GJ. Decrease in Trunk Muscular Response to Perturbation with Preactivation of Lumbar-Spinal Musculature. Spine 2000;25:1957-1964.
- Cholewick J, McGill SM, Norman RW. Lumbar spine loads during lifting extremely heavy weights. Medicine and Science in Sports and Exercise 1991;23(10):1179-1186.
Craig Liebenson,
DC Los Angeles, California
cldc@flash.net



