It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
The Not-So-Hidden Costs of Back Pain
The research findings are well-documented, and your clinical experiences undoubtedly verify it: Back pain affects nearly everyone. An estimated 80 percent of adults experience one or more episodes of back pain in their lifetime,1,2 and the one-year prevalence rate is approximately 15%-20%, with some estimates as high as 40%.3 However, some "experts" - ironically, those outside the chiropractic profession - have attempted to describe back pain as a harmless, self-limiting condition that requires only rest and time for resolution, despite evidence to the contrary.4
If that's the case, how do these experts explain the results of a study5 published in the Jan. 1, 2004 issue of Spine? "Estimates and Patterns of Direct Health Care Expenditures Among Individuals With Back Pain in the United States" analyzed data from the 1998 Medical Expenditure Panel Survey (MEPS), a national survey on health care utilization and expenditures. Researchers utilized data from the MEPS for two specific purposes: to estimate U.S. health care expenditures for back pain in 1998 and to describe health care expenditure patterns among individuals with back pain during that time period.
Study Parameters
The study population included survey respondents ages 18 and older. Back pain was defined as pain experienced in all back areas and including any back disorders, disc disorders and back injuries. International Classification of Disease - 9th Edition (ICD-9) codes utilized to identify back pain patients included 720-724, 805-806, 839, and 846-847. The most common back diagnosis was 724, which includes spinal stenosis, lumbago, sciatica, and other unspecified back disorders. Other common diagnoses included 847 (back strains and sprains), 722 (disc disorders) and 723 (other disorders of cervical region).
According to the 1998 MEPS, which used data from a sampling of the U.S. population to estimate national prevalence rates, 2,120 adult respondents - representing an estimated 25.9 million U.S. adults - reported suffering back pain at "some time" in 1998.
Health care expenditures were defined as the sum cost of direct payments for care provided in 1998. Any costs for uncompensated care were not included. Health care expenditures included out-of-pocket payments and payments by private insurance, Medicaid, Medicare, workers' compensation, and other sources.
Estimates for health care expenditures included costs associated with inpatient care, outpatient care, office-based visits, emergency room visits, prescription drugs, home health services, dental care, vision aids, and medical equipment purchase. Office-based and outpatient services included visits to medical physicians, chiropractors, physical therapists, psychologists, occupational therapists, nurses and nurse practitioners, social workers and physician's assistants.
Results
- Estimated total health care expenditures for back pain sufferers were a staggering $90.7 billion in 1998. Expenditures for inpatient care accounted for the largest proportion of total expenditures ($27.9 billion), followed by office-based visits ($23.6 billion).
- Prescription drugs accounted for more than 15% of the total health care expenditures ($14.1 billion) incurred by back pain sufferers. By the authors' best estimates, drug expenditures accounted for greater than 10% of total incremental expenditures - a substantial jump compared to previous research that estimated drug expenditures at less than 1% of all costs for back pain. The authors note that prescription drug expenditures for back pain have increased more rapidly than any of the other service expenditures.
- Health care expenditures were not equally distributed: "For each health service, the 10% most expensive individuals accounted for >50% of the service expenditures. The 25% most expensive individuals accounted for >75% of the service expenditures. ... This pattern was particularly clear for inpatient care, outpatient services and emergency room visits."
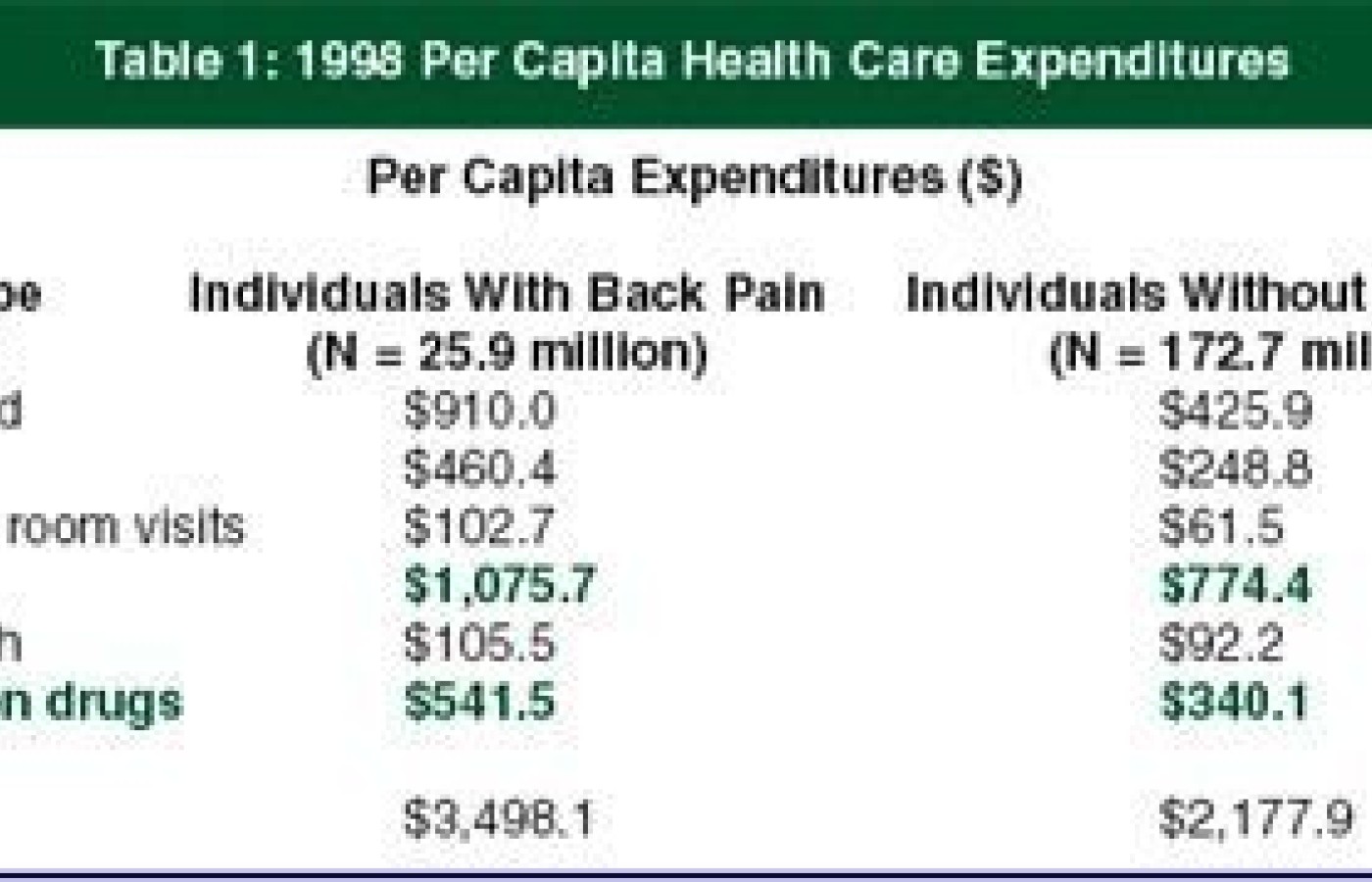
- Average health care costs incurred by individuals with back pain were approximately 60% higher than those without back pain. These average costs were determined by summing overall health care expenditures, then dividing total expenditures by the number of individuals in each group (individuals with back pain and individuals without back pain) to estimate total health care expenditures per person in the U.S. in 1998. (See Table 1.)
If these data aren't troublesome enough, the authors note that their estimates may be understated, as they did not include costs associated with nursing home care, which accounted for approximately 20% of total health care costs for back pain in previous studies. Additionally, the ICD-9 codes utilized to define back pain in the MEPS were limited to three-digit codes, with no subclassifications.
The bottom line: Health care costs attributable to back pain in 1998 were "substantial," according to the authors, and demonstrate "wide variation among back pain individuals with different clinical, demographic, and socioeconomic characteristics." One can only assume that in 2004, these figures are notably higher, both in terms of the number of people suffering from back pain and the associated health care costs.
For doctors of chiropractic, this study reinforces what you've been saying all along: Back pain affects a significant percentage of the population, and when not treated appropriately, it can account for substantial health care costs - particularly in terms of prescription drugs and hospital visits. And lead researcher Xuemei Luo makes perhaps the most important point, noting that chronic back pain cases usually account for the biggest expenditures, including doctor visits, prescription drugs, and overall health services.6
References
- Frymoyer JW, Cats-Baril WL. An overview of the incidences and costs of low back pain. Orthop Clin North Am 1991;22:263.71.
- Pain, disability, and satisfaction outcomes and predictors of outcomes: a practice-based study of chronic low back pain patients attending primary care and chiropractic physicians. JMPT September 2001;24(7):433-9.
- Papageorgiou AC, Croft PR, Ferry S, et al. Estimating the prevalence of low back pain in the general population. Spine 1995;20:1889-94.
- Hagen KB, Hilde G, Jamtvedt G, et al. The Cochrane review of bed rest for acute low back pain and sciatica. Spine 2000;25(22):2932-39.
- Luo X, Pietrobon R, Sun SX, et al. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine 2004;29(1):79-86.
- Back pain takes big toll on U.S. health dollar. Total medical costs likely top $100 billion a year. HealthScout, Jan. 2, 2004.
Peter W. Crownfield, managing editor