It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Low Back Pain: A Case History
A study1 in the February 2001 New England Journal of Medicine reported that 85 percent of all low back injuries could not be accurately diagnosed pathoanatomically. The study noted three areas of concern that physicians should consider:
- Is the pain due to a systemic disorder?
- Is the pain due to a social or psychological issue?
- Is the pain due to discogenic involvement necessitating surgery?
This narrowed perception of the cause of low back pain drastically reduces the opportunity for a physician to fully understand what really is the cause in most episodes of low back pain. Coach Tony Tullock is one of many athletes victimized by such nearsightedness for almost 10 years.
At the age of 17, Tony suffered a severe hyperextension injury to his lower back while playing hockey. For 10 years he sought help from many sources. Unfortunately, his results were limited, as the approach taken was similar to the information in NEJM. All his physicians were looking for was pathology while ignoring biomechanics, which was the cause of Tony's problem. Despite being the head strength and conditioning coach of a Division I program, and that Tony was responsible for 430 Division I athletes, he continued to suffer severe low back pain, limiting him greatly in his abilities to demonstrate correct exercises to his athletes, and affecting his personal life and workouts.
Tony's History
Tony, 27, came to my office in early May of this year. For a decade he had been unable to get answers for his condition. As a strength coach, he found it hard to explain why he was unable to demonstrate many of his exercises. He'd been treated a few times by a chiropractor 10 years earlier with limited results. An MD had x-rays and an MRI performed, but they were negative. Tony continued looking for anyone to give an opinion on his problem. He saw several more MDs, who all prescribed medications, and prior to seeing me, his activities and exercises were guarded.

The Structural Exam
The goal here was to look at this athlete from a structural point of view. No one, to date, had looked at him this way, which suggested that his condition could be attributed to structural imbalances and distortions.
Upon examination, I looked at Tony's feet. He clearly had problems in the medial arches. The right foot was pronated; the left appeared to have a normal medial arch. This was the foundation of imbalance, and would most likely be part of the cause of his problems. Associated with this distortion pattern, Tony had an increased Q-angle on the right, while the left Q-angle was normal (Figure 1). There was pain on flexion during (lumbosacral) range of motion, while all other positions were normal. The toe-in test, done passively with the patient in a supine position, showed a greater internal rotation on the left than the right. A Patrick-Fabere test on the right was positive, as was Lasegue's. Leg lengths were even at 31 1/2 inches.
X-ray Findings
I explained to Tony that standing x-rays showed 75 percent of all the structural findings we were looking for. As a preliminary precaution, four x-rays would be taken; if necessary, additional ones would be taken. We started with an A-P open mouth, a lateral cervical, an A-P L-S and a lateral L-S.

On Tony's x-rays, there were many subtle findings, but the lateral L-S showed more than enough reason for his 10 years of problems. A normal sacral base angle (Figure 2 on page NE-2) would be 36Á-42.Á Tony's lateral L-S (Figure 3) had a 56Á sacral base angle. In addition to this distortion, he also had a severe anterior gravity line. Normal weightbearing should bisect the anterior third of the sacral base.
Recommendations
Tony was suffering from a severe imbalance in the L-S and pelvic alignment. This distortion created abnormal stress on areas of the low back that were not designed to handle the stress, yet no one had detected this previously. Now that it had been detected, a corrective program could be outlined. The first objective was to fit him for custom-made orthotics, as his foundation was imbalanced. I use a weightbearing impression, vs. a neutral casting method. I also recommend a softer (instead of a rigid) orthotic. This is a critical part of the program, as all structural balance originates with the feet.
In my office, we've developed an "advanced conditioning" program. This is a six-month program, consisting of 40 adjustments:
- three times a week for six weeks;
- twice a week for six weeks;
- once a week for six weeks; and
- once every two weeks for eight weeks.
Also included are trigger point therapies, ultrasound treatments, and a six-month exercise program designed by my office's personal trainer. The exercise program design is based on the patient's objectives, the structural distortions that are present, and the progression of exercising our personal trainer has outlined.
Due to Tony's position as a Division I head strength coach, he elected not to enlist in our exercise portion of the program. He felt he could orchestrate a program for himself. When we work with a patient on the exercise phase of the program, our goal is to assess the patient for strengths and weaknesses in the core muscles, and the low back muscles. Strength, stability, and flexibility of all parts of the body are goals we set for patients.
We also implemented a program with Tony that allowed him to use a special trigger points stick to maximize benefits. The stick allows a patient to increase blood flow to repetitively used muscles, while also reducing tension and toxin build-up in the muscles. Tony immediately saw improvements in his back pain once he started this phase of the program.
Tony was the perfect patient, because he understood that structural change would take time and hard work. He also understood that distortions in his feet would impact the low back and the rest of the body.
The key to success here is to develop the means to have a patient come in enough times over a reasonable period of time to get the objective changes that are needed. In this confusing managed care and insurance-based climate, so many patients are unable to make correct decisions about the type and amount of care they need. Our advanced conditioning program clearly outlines that six months of continual care is needed to begin to make the structural changes to improve an athlete's future.

Re-X-raying
About 10 weeks into the program, Tony said his low back felt "different." He could do more activities with his low back than he used to, and was slowly developing the confidence to do things he had been afraid to do over the past 10 years. We talked about the possibility of re-x-raying him. I usually wait a full six months before I consider re-x-raying a patient, however, due to his youth, his job, and his interest in learning if there were any objective changes in the x-rays, I re-x-rayed him.
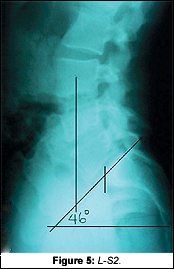
The new x-rays showed significant changes to the neck and low back. The most obvious and most important was the change on the lateral L-S. Tony's sacral base angle went from 56Á to 46Á (Fig. 5). Knowing that normal is 36Á-42Á, this improvement was tremendous. Tony demonstrated many improved findings on his functional re-examination as well.
Conclusion
Here we have a coach/athlete who is responsible for training Division I athletes. He is clearly knowledgeable of conditioning, but highly frustrated at the conventional system that addresses sports injuries as pathological problems. Most injuries are structural, and until we develop a system of testing, treating, and of re-examining the athlete, we won't succeed in advancing in the sports medicine arena.
Today, Coach Tony Tullock performs many exercises he couldn't previously, because he stepped out of the traditional system available to athletes. As chiropractors, we need to alert athletes in our communities to the possibilities of proactive care vs. reactive care. And with proper examination and conditioning programs, all athletes can reach a higher level of balance and performance in structural function.
Chiropractors are in the best position to step up and become the sports injury specialists in their communities. It is a continual process in developing this system in the office and educating the community of the difference in your work vs. others, but the benefits are so huge, the price you pay is worth it.
Reference
- Deyo R, Weinstein J. Primary care: low back pain. New England Journal of Medicine Feb. 1,2001:344(5);363-370.
Tim Maggs,DC
Schenectady, New York



