It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Debunking the Myth of Surgical Necessity
- A systematic review investigated the theory that spondylolysis with or without isthmic spondylolisthesis (spondylolysis/spondylolisthesis) causes low back pain.
- The researchers found no consequential association between spondylolysis/spondylolisthesis and low back pain.
- Conservative treatment is effective for most patients with spondylolysis/spondylolisthesis, focusing on recovery of function, mobility, and pain control through therapeutic exercise, manipulation/mobilization, and other physical therapies.
A new patient brings in an X-ray, revealing a spondylolisthesis. The patient says a spinal surgeon told her the cause of her low back pain is spondylolisthesis and recommended spinal fusion surgery.
What is your response? What does the current research demonstrate? Today, I present a systematic review that investigates the theory that spondylolysis with or without isthmic spondylolisthesis (spondylolysis/spondylolisthesis) causes low back pain.
This study was published in the European Spine Journal, an evidence-based, peer-reviewed journal.1 The research team consisted of four medical doctors and one PhD who thoroughly searched for published studies that investigated the association between spondylolysis/spondylolisthesis and low back pain in adults. After evaluating the methodological quality of the studies, they found 15 studies with reasonable research quality, representing 9,291 patients.
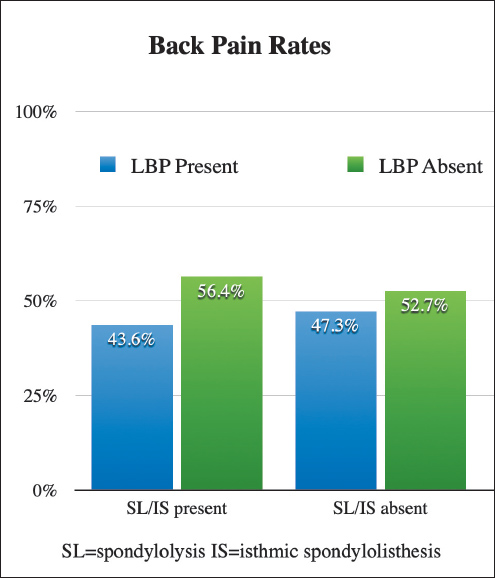
The graph titled “Back Pain Rates” demonstrates the conclusions of this study. The researchers found no consequential association between spondylolysis/spondylolisthesis and low back pain. Spondylolysis/spondylolisthesis coexists with and without low back pain at very similar rates. In general, spondylolysis/spondylolisthesis is an incidental finding.
Previous research supports these findings. Beutler and colleagues provide perhaps the most definitive evidence to date on the natural history of spondylolisthesis.2 This research team identified young subjects with spondylolisthesis. Over a 45-year follow-up period, these subjects reported no difference in pain, disability, or quality of life compared to the general population.
Surgical Management
Over 50,000 patients in the U.S. each year have spinal surgery for spondylolisthesis, costing over $35,000 per surgery.4 The harms associated with this surgery are serious and numerous. Pseudoarthrosis rates are above 20%, the re-operation rate is 10%, and the incidence of neurological issues is estimated at 45%.3,9
The surgical treatment of spondylolisthesis is largely based on tradition. The surgery was popularized in the 1930s based on a theory, but without evidence.8 To this day, there are no quality RCTs demonstrating the long-term benefits of this surgery. The preponderance of scientific research demonstrates a lack of evidence for the surgical approach.
The largest and most prestigious society of spinal doctors and surgeons is the North American Spine Society, and its discovered and published the following: There is insufficient evidence to make a recommendation for the efficacy of surgical treatment as compared to medical/interventional treatment alone for the management of adult patients with spondylolisthesis.5
Conservative Management
Conservative treatment is effective for most patients with spondylolysis/spondylolisthesis.6 Primary conservative procedures focus on the recovery of function, mobility, and pain control through therapeutic exercise, manipulation/mobilization, and other physical therapies.7,10
In light of the benign natural history demonstrated by Beutler and colleagues, and the lack of association between spondylolysis/spondylolisthesis and low back pain in this current systematic review, surgery should be avoided. Based on current research, there is no causal relationship between spondylolysis/spondylolisthesis and low back pain, and there is no justification for surgery for this condition.
Time for a Medical Reversal
When scientific research discredits the use of outdated or unproven practices, those practices need to be discontinued. In the case of surgery for spondylolysis/spondylolisthesis, it is time for a medical reversal. Spinal surgeons should immediately stop performing these surgeries.
Scientific evidence currently supports a conservative approach because it is effective and has a very good safety profile. Conversely, surgery lacks evidence that it is better than a conservative approach, and it is clearly associated with numerous serious harms.
The loud and clear recommendation for our profession is that we stop referring spondylolysis/spondylolisthesis cases to spinal surgeons, except in progressive neurological situations (cases that have bowel or bladder incontinence). Instead, we should manage these cases ourselves.
References
- Andrade NS, Ashton CM, Wray NP, et al. Systematic review of observational studies reveals no association between low back pain and lumbar spondylolysis with or without isthmic spondylolisthesis. Eur Spine J, 2015;24:1289-95.
- Beutler WJ, Fredrickson BE, Murtland A, et al. The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Spine, 2003;28:1027-1035.
- Chen Y, Zhou Y, Chen J, et al. A systematic review and meta-analysis of risk factors for reoperation after degenerative lumbar spondylolisthesis surgery. BMC Surg, 2023;23:192.
- Greenberg JK, Olsen MA, Dibble CF, et al. Comparison of cost and complication rates for profiling hospital performance in lumbar fusion for spondylolisthesis. Spine J, 2021;21:2026-2034.
- Kreiner DS, Baisden J, Mazanec DJ, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of adult isthmic spondylolisthesis. Spine J, 2016;16:1478-1485.
- Leonidou A, Lepetsos P, Pagkalos J, et al. Treatment for spondylolysis and spondylolisthesis in children. J Orthop Surg (Hong Kong), 2015;23:379-82.
- Liu Z, Qin X, Sun K, et al. Manipulation for degenerative lumbar spondylolisthesis: a systematic review of randomized controlled trials. J Trad Chin Med Sci, 2022;9:121-127.
- Meyerding HW. Spondylolisthesis. J Bone Joint Surg (Am), 1931;13:39-48.
- Ruparel S, Chaddha R. Complications in spondylolisthesis surgery: common, uncommon, and rare. Ind Spine J, 2021;4:77-88.
- Vanti C, Ferrari S, Guccione AA, et al. Lumbar spondylolisthesis: STATE of the art on assessment and conservative treatment. Arch Physiother, 2021;11:19.



