It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Dead Butt: Gluteal Amnesia
- Even people who are active and exercise on a regular basis can be at risk for developing gluteus medius problems.
- No matter what term we use to describe this condition, it can be easily managed with chiropractic care.
- Once the diagnosis is determined, this condition can be managed conservatively with patient education and gluteal activation exercises.
Gluteal amnesia, AKA dead butt syndrome or dormant butt, has become an increasing problem over the past decade. The term dead butt seems to have gotten the public’s attention more than gluteal amnesia or dormant butt. Other terms for the same condition are gluteus medius syndrome, gluteus medius tendinosis and lower crossed syndrome. I personally prefer lower crossed syndrome, coined by Valdimir Janda.
Clinical Presentation
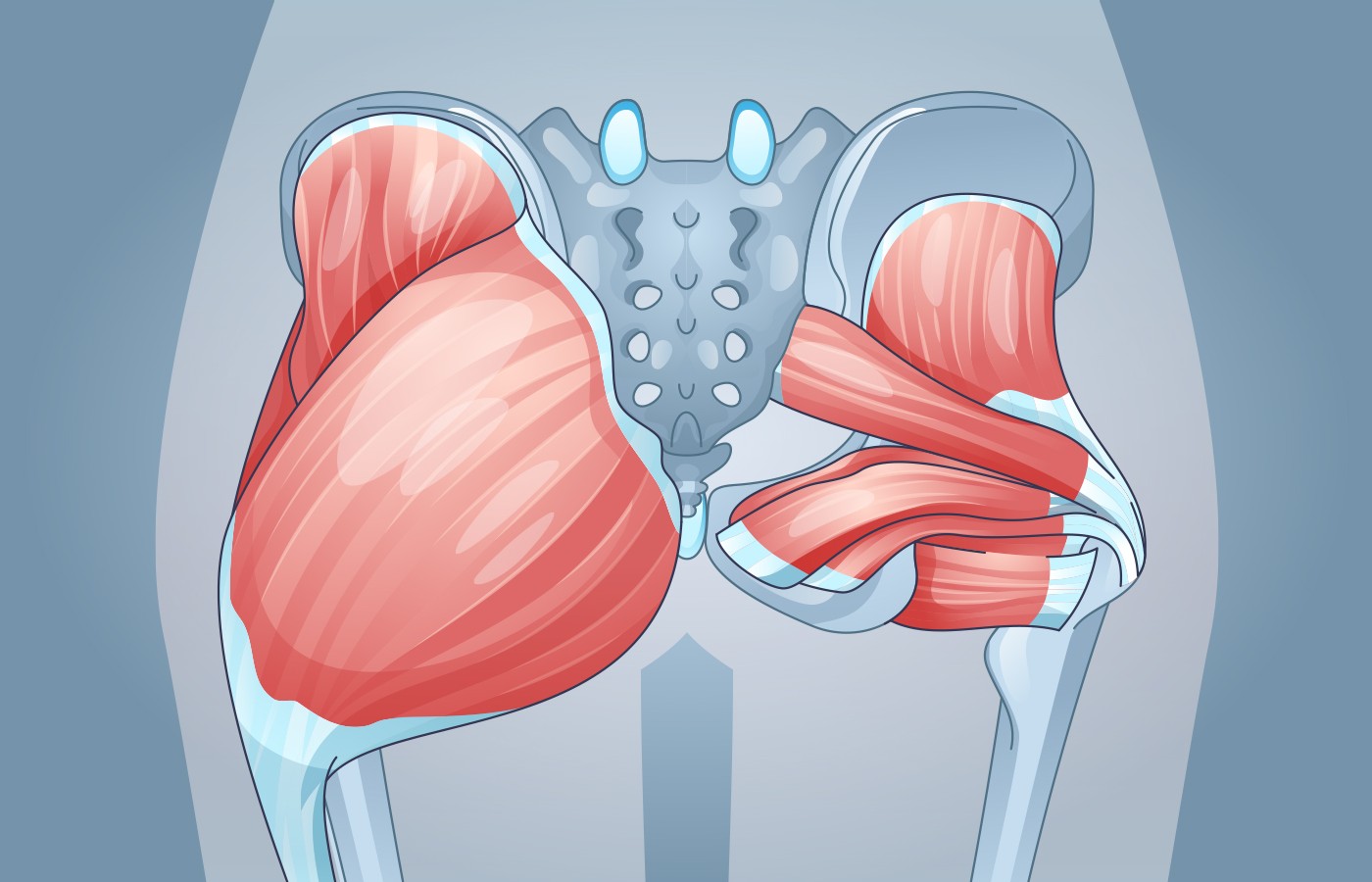
Lower crossed syndrome1 is characterized by specific patterns of muscle weakness and tightness that cross between the posterior and the anterior sides of the body. In LCS there is overactivity of the hip flexors hip and lumbar extensors; and underactivity and weakness of the deep abdominal muscles and of the gluteus maximus and medius.
This imbalance results in an anterior tilt of the pelvis increased flexion of the hips, and compensatory hyperlordosis in the lumbar spine. With the hip flexors tightened, and the glutes inhibited, over time the glutes are less likely to fire properly and work efficiently.
If not corrected, the symptoms of stiffness and pain can afftect the glutes, hips, lower back, and knees. Some patients even experience sciatic radiculopathy. Pain may force a change in their gait (Trendelenburg gait). Of course, frequently the patient will have a positive Trendelenburg test.
Even people who are active and exercise on a regular basis can be at risk for developing gluteus medius problems. Despite several hours a week exercising, if one sits for hours at a time most of the day without breaks, this condition can occur.
(Tiger Woods famously pulled out of a golf tournament because of gluteal amnesia.)
Differential Diagnosis
The issue is how to differentiate this condition from other musculoskeletal conditions involving the hip and lower back. With myofascial buttock pain in adults, gluteal tendinopathy, greater trochanteric tendinopathy and iliotibial band thickening along with weak gluteal muscles are common. One should also consider the lumbar spine, the hip joint, sacroiliac joint pathology, piriformis syndrome, and proximal hamstring tendinopathy, but there certainly can be some overlap.2
After a thorough history and physical examination (which are beyond the scope of this article; to review, try this link: http://askdrlehman.com/UBDX612/hip26.pdf), if the patient has a history of a sport-related activity or has a possible underlying condition, such as osteoporosis, then plain films of the pelvis are recommended. If the source of the symptoms is myofascial, plain films will be unremarkable.
Advancements in magnetic resonance imaging (MRI) have broadened the differential diagnosis of pain around the hip joint and buttocks to include trochanteric bursitis, tendinopathy of the gluteal muscle, and iliotibial band and hamstring tears. MRI can distinguish between extra-articular and intra-articular causes of hip pain in patients.
MSK ultrasound as an adjunctive tool can also be helpful in pinpointing the problem. Ultrasound of the hip shows tendon thickening with loss of normal fibrillar pattern with hypoechoic fluid. Bursitis, on the other hand, is defined as an anechoic fluid collection in the expected location of either the greater trochanteric bursa or sub gluteus medius bursa.3-5
Once the diagnosis is determined, this condition can be managed conservatively with patient education and gluteal activation exercises. The need for more aggressive treatment is generally unwarranted, especially if the patient is willing to participate in the therapy.6
Chiropractic Management
No matter what term we use to describe this condition, it can be easily managed with chiropractic care. Many chiropractors even advertise this condition to prospective patients.7 The important point is to confirm this diagnosis before beginning treatment, since this syndrome can present as an athletic injury or develop over time as result of physical inactivity. Plain films of the pelvis should rule out most osseous trauma, but if patient does not respond to conservative care, MRI or even MSK ultrasound should be able to diagnose any significant tendinopathy or bursitis.
Adult working-class Americans spend on average 50% of their awake time at work, be it on site or remote. Moreover, more than 80% of jobs in the U.S. involve mostly sedentary activities,8 which results in daily long sitting hours and a colossal work-related lifetime of physically inactive behaviors.9-10
According to the Mayo Clinic,11 an analysis of 13 studies concluded that, “sitting time and activity levels found in those who sat for more than 8 hours a day with no physical activity had a risk of dying similar to the risks of dying posed by obesity and smoking.”
The more we sit, the less we use our muscles. Sitting causes some muscles to tighten and shorten and others to stay stretched and inhibited, leading to biomechanical imbalance. Appropriate education of the patient is key to appropriate recovery.
Always take time to explain the problems to patients so that they understand why different issues are affecting them. Chiropractors are very good at communication and explaining to patients what is wrong and how they can help to resolve it.
Chiropractors also know how to manage gluteus medius syndrome or dead butt syndrome. I am not going to go into any detail except to remind you of the exercises that commonly help this condition.
- Double-leg bridge
- Single-leg bridge
- Clam
- Abduction lifts with foot inverted
- Hip extensions
Of course, you can add weights or resistance bands depending on the patient’s ability.
References
- Key J. The Pelvic crossed syndromes: a reflection of imbalanced function in the myofascial envelope; a further exploration of Janda’s work. J Bodyw Move Ther, 2010 July;14:299-301.
- Battaglia PJ, D’Angelo K, Kettner NW. Posterior, lateral, and anterior hip pain due to musculoskeletal origin: a narrative literature review of history, physical examination, and diagnostic imaging. J Chiropr Med, 2016 Dec;15(4):281-293.
- Sunil Kumar KH, Rawal J, Nakano N, et al. Pathogenesis and contemporary diagnoses for lateral hip pain: a scoping review. Knee Surg Sports Traumatol Arthrosc, 2021 Aug;29(8):2408-2416.
- Saad A, McLoughlin E, Kalia SS, et al. Gluteus medius muscle pathologies - a case series & pictorial review. J Orthop, 2020 Mar 28;21:270-274.
- Chamberlain R. Hip pain in adults: evaluation and differential diagnosis. Am Fam Physician, 2021 Jan 15;103(2):81-89. Erratum in: Am Fam Physician, 2021 Mar 1;103(5):263.
- Mellor R, Bennell K, Grimaldi A, et al. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. Br J Sports Med, 2018 Nov;52(22):1464-1472.
- Bertelsman T. “Two Hip Pain Mistakes All Chiropractors Must Avoid.” ChiroUp.com, April 28, 2021.
- “What Percentage of Americans Work Desk Jobs?” TheDesiredDesk.com, Aug. 8, 2021.
- Church TS, Thomas DM, Tudor-Locke C, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One, 2011;6(5):e19657.
- Duffy EY, Hiremath PG, Martinez-Amezcua P, et al. Opportunities to improve cardiovascular health in the new American workplace. Am J Prev Cardiol, 2020 Dec 8;5:100136.
- Laskowski ER. “Sitting Risks: How Harmful Is Too Much Sitting?” The Mayo Clinic.