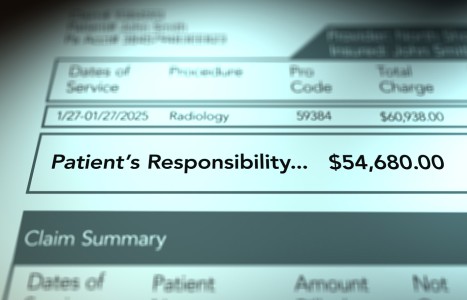
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Lumbar Instability: The Case of the Missing Spondylolisthesis
Review the routine radiograph in Figure 1A [left image]. The patient has a spondylolisthesis at L4-L5. Now review the MR image of the same patient in Figure 1B [right image]. Where did the spondylolisthesis go? The answer? Instability allowed the spondylolisthesis to reduce.
The routine radiograph was taken with the patient standing, bearing his body weight. In that position, gravity assists the unstable L4 segment in moving anteriorly. The MR scan was taken with the patient supine, bearing a much lower degree of body weight. Gravity is less of a factor here, and the L4 segment moves posteriorly, closer to its normal position.
Clues to Instability
In cases such as this, it is not unusual for the patient to report that they feel the shift of the unstable segment when transferring from one posture to another. This information is a crucial clue to instability when reported by the patient during the case history. The sensation will be described as a "deep clunk," a feeling differing from the sensation associated with typical joint cavitation.
In the initial stages of a case, when routine radiographs may or may not be taken, it is difficult to identify this degree of instability, much less smaller instabilities. These situations are a problem.
If no radiographs are taken initially, the spondylolisthesis will not be identified; neither will the instability. If radiographs are taken initially, only the spondylolisthesis will be identified. Instability can be assumed, but the degree of instability cannot be accurately assessed.
Radiographic Recommendation
Flexion and extension views are often used to assess spinal instabilities. However, there is an additional recommendation here.
From reviewing the images in Figures 1A and 1B, common sense would suggest that when a spondylolisthesis is identified on a standing lateral view, an additional lateral view taken with the patient supine could be helpful. The goal is to detect the transition of the unstable segment, similar to the transition seen in Figures 1A and 1B.
The view could be a spot view of the area in question. The second lateral will be quick to obtain and does not require a trial course of care or precertification.
One procedural issue with the recumbent lateral must be addressed with this recommendation. An MR scan requires much more time to perform than a recumbent lateral radiograph. With the MR, the patient is recumbent for a considerable time before imaging begins. The transitioning of the unstable segment will have time to occur. Transitioning of the unstable segment may not have enough time to occur before the routine radiograph is recorded.
To compensate for this, the patient should lie in the recumbent position for several minutes before recording the second lateral radiograph.
Orthopedic Recommendation
Another option for identifying instabilities, one possibly performed before imaging, is orthopedic testing. While much less accurate, orthopedic testing is fast, adds minimal time to the course of an examination, and does not involve radiation and additional expense. Three orthopedic tests are recommended: the shopping cart sign, the prone instability test and Milgram's test.
The shopping cart sign is actually more of a history finding than a test. During the case history, when the patient is quizzed about the postures and activities that exacerbate and relieve symptoms, the patient with stenosis will often report lower-extremity symptoms that develop while waking. These symptoms can be relieved by sitting or leaning over a shopping cart.
The shopping cart sign can be present with stenosis created by instability. It can also be present with stenosis created by other pathologies – one of the reasons for mentioning the inaccuracy of some orthopedic tests.
The prone instability test is performed with the patient kneeling on the floor, torso lying over a chair or low exam table. It can also be performed with the patient standing with the torso lying on a tall examination table.
In the first method, the examiner palpates the individual lumbar segments, assessing for tenderness. If segments are identified as tender, the patient is asked to raise their feet off the floor. The maneuver contracts the lumbar extensor musculature. The isometric contraction stabilizes the lumbar region.
The segments identified as tender earlier are reassessed during the isometric contraction to determine if they are still tender. Segments that are no longer tender are believed to be unstable.
In the second method, after the initial palpation of lumbar segments, both legs are lifted to create contraction of the lumbar extensor muscles. Everything is the same as the first method from that point.
For Milgram's test, the patient is instructed to lift both legs and hold them a few inches above the table. The position is held for at least 30 seconds. Pain in the lumbar area indicates the probability of instability.
A note of caution is necessary regarding the interpretation of Milgram's. Patients with week abdominal muscles may not be able to perform the test. The isometric contraction of abdominal muscles may increase intra-abdominal and intradiscal pressures, possibly re-creating the symptoms of a space-occupying lesion. Lumbar facet syndromes can be aggravated during the test. These are essential differential diagnosis factors and yet another reason for being aware of the accuracy or inaccuracy of many orthopedic tests.
Clinical Takeaway
The importance of this case and other cases like it points to safety concerns for the patient. Manipulation of an unstable area, as is depicted here, is contraindicated. Referral for a second opinion for the unstable area is necessary, as the area will likely require surgical stabilization.
Adjusting other areas of the patient's spine is permissible if those areas are stable. The patient can still benefit from chiropractic care, with caution employed.
Resources
- Magee DJ. Orthopaedic Physical Assessment, 5th Edition. Saunders-Elsevier, 2008.
- Wong DA, Transfeldt E. McNab's Backache, 4th Edition. Lippincott, Williams and Wilkins, 2007.
- CORE, Clinical Orthopaedic Exam: a diagnostic utility and reference tool for musculoskeletal disorders. Clinically Relevant Technologies, 2010.