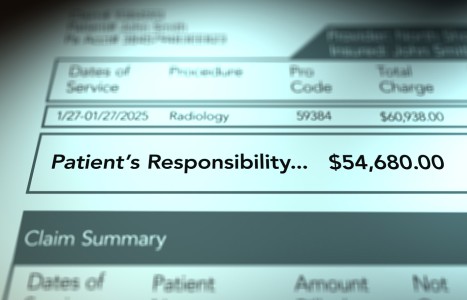
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Our Wasted Opportunity
Normal-weight people who never exercise tend to be overfat and hyperglycemic, which is why they can be metabolically obese1-4 and thus chronically inflamed, just like overtly obese individuals who are hyperglycemic. To date, no health care profession has effectively and properly delivered the obesity / hyperglycemia and chronic inflammation message to the general public. Why could it not come from our chiropractic colleges, organizations, and associations?
Inflammation and Viral Infections
The reason why the body chemistry of obesity and hyperglycemia promotes viral infections [See Dr. Seaman's column in the January issue] is because the chronically inflamed obese / hyperglycemic body is unable to effectively respond to and eliminate a viral infection. The easiest way to identify one's prevailing inflammatory state is to test for high sensitivity C-reactive protein (hsCRP), which generally rises with increasing body fat and rising blood glucose levels.
A normal level of hsCRP is less than 1 mg/L. Between 1 and 3 mg/L is considered to reflect mild inflammation. The average middle-aged American has a hsCRP of 1.5 mg/L. It is estimated that 25 percent of the U.S. population have hsCRP levels over 3 mg/L, which reflects a state of moderate to high inflammation. I like hsCRP because it generally mirrors pro-inflammatory cytokine levels, which correlate to the potential severity of a viral infection. Notice the title of this article:
Lieu Q, Zhou Y, Yan Z. The cytokine storm of severe influenza and development of immunomodulatory therapy. Cell Mol Immunol, 2016;13(1):3-10.
Connecting the Dots: Cytokines and Inflammation
The term cytokine storm refers to an excessive overproduction of cytokines, which can have lethal effects. The cytokine storm was known to be an issue for severe flu sufferers and the same was discovered for people with severe cases of COVID.
Cytokine is the name given to a family several dozen proteins, the most notable group are called interleukins, of which there are more than 30. Most cytokines are pro-inflammatory, such as interleukin-1 (IL-1), interleukin-6 (IL-6), interleukin-17 (IL-17), and tumor necrosis factor (TNF).
Cytokines are released by cells when they are stressed. After the stressor resolves, cytokine levels are supposed to go back to normal. A cytokine storm refers to an excessive release of cytokines that subsequently damages the body or leads to death. In "storm language," a cloudy, drizzly day can be likened to "catching a cold" and feeling under the weather for a few days. The cold symptoms were created by a mild elevation in the production of cytokines and other inflammatory chemicals. In contrast, a cytokine storm is like a tornado or hurricane that rips a town apart, causing death and destruction.
Over the past 20 years, scientists have discovered that overt trauma is not necessary to cause cells to increase their release of cytokines at a sustained chronic low level. Chronic mental / emotional stressors events, sedentary living, chronic sleep loss, and a pro-inflammatory diet can cause cells to release an excess of cytokines. Even minor acute stressful events can cause cytokine release, such as eating several donuts in one sitting or missing a night's sleep. We should view these as low-grade cumulative stressors.
Most people who suffer from too many years of exposure to chronic stressors and the subsequent lifestyle-induced chronic inflammation will likely develop a chronic inflammatory disease, such as chronic pain, depression, diabetes, hypertension, heart disease, cancer, Alzheimer's disease and/or other chronic diseases. It is important to understand that these various diseases manifest because people are chronically living in an elevated cytokine state. So, it should not be surprising that when some of these people are infected by a virus, they will suffer from a lethal cytokine storm.
Chronic Inflammation: The Perfect Focus for Chiropractic
There is historical precedence for the chiropractic profession to focus on reducing chronic inflammation. In a 1914 book titled The Chiropractor (pg. 27), D.D. Palmer wrote that "inflammation is present in most, if not all diseases, in the acute if not the chronic." Cumulative stressors gradually increase inflammation over time, which causes certain people to become too inflamed to effectively respond to adjustments and rehabilitation efforts, no matter if you believe in subluxations or mechanical back pain.
In other words, no matter if one is the most metaphysical of all subluxation-based chiropractors or the most allegedly scientific of all mechanical back pain chiropractors, the common enemy of treatment success is chronic inflammation.5-7
Unfortunately, chronic inflammation is mostly not an issue of concern for the chiropractic profession. If it was, students would graduate from our colleges knowing the biochemical relationships among obesity, hyperglycemia, chronic inflammation, chronic pain, osteoarthritis, tendinopathy, disc herniation, and osteoporosis. All DCs would also know how to answer the question posed in the title of this article:
Conaghan PG, Vanharanta H, Dieppe PA. Is progressive osteoarthritis an atheromatous vascular disease? Ann Rheum Dis, 2005;64:1539-41.
If all chiropractors knew osteoarthritis is biochemically similar to atherosclerosis, no chiropractor would be surprised that only about 12 percent of all osteoarthritis cases are caused by overt joint injury.8 Similarly, if all chiropractors knew tendinopathy is biochemically similar to atherosclerosis, no chiropractor would be surprised that tendinopathy researchers have suggested we view chronic tendinopathy as a cardiovascular disease.9
Research has also demonstrated that the same lifestyle-induced chronic inflammation which causes atherosclerosis also causes muscles to degenerate, bones to develop osteoporosis and discs to herniate.10
It is important to understand that when you read the words cardiovascular disease or atherosclerosis, you are actually reading lifestyle-induced chronic inflammation of arteries that is caused by cumulative stressors. This also means that when you think of osteoarthritis, tendinopathy, osteoporosis, muscle atrophy, and disc herniation, you should be understanding these conditions to be "lifestyle-induced chronic inflammation of joints, tendons, muscles, bones, and discs" that are caused by the same cumulative stressors.7
Inflammation and Musculoskeletal Degeneration
Hopefully it is obvious that understanding the relationship between lifestyle-induced inflammation and musculoskeletal degeneration is extremely useful for managing patients with chronic musculoskeletal conditions.
First, it should be applied to patients who do not respond adequately to manual care and rehabilitation. These patients should be told to reduce their cumulative stressors at least to a level that reduces inflammation enough so they respond to chiropractic manual and rehabilitation treatments.
Second, it should be applied to all patients as a disease-prevention strategy. All patients should know that all people have a chronic inflammation threshold that needs to be avoided so patients can respond well to chiropractic treatments and also avoid the development of chronic inflammatory disease, the most notable being heart disease and cancer.
Chiropractic's Missed Opportunity
To be clear, it is very simple to track lifestyle-induced inflammation, which should include at least hsCRP, vitamin D, body mass index, waist/hip ratio, and the metabolic syndrome markers, which include fasting glucose, triglycerides, HDL cholesterol, blood pressure and waist circumference. In order to be diagnosed with the metabolic syndrome, 3/5 criteria must be present. By tracking these markers, you would know if someone is not inflamed or has mild, moderate, high, or severe chronic inflammation.
As stated above, the more severe the inflammation, the less likely a patient is to respond to chiropractic manual and rehabilitation treatment methods. Similarly, the more the severe the inflammation, the more likely one is to develop a cytokine storm if infected with the flu or coronaviruses.
To date, no health care profession has taken the position that we as a nation need to get healthy to overcome our current COVID dilemma, which is shocking to me as more than 100 years, ago D.D. Palmer knew chronic inflammation was a key clinical issue for patients to overcome.
If chiropractors were trained to habitually track the basic inflammation markers discussed above for the purpose of identifying patients at risk of not responding to chiropractic care, this could have easily been applied to patients at risk of having a catastrophic COVID outcome.
References
- Ruderman NB, Schneider SC, Berchtold P. The "metabolically obese," normal-weight concept. Am J Clin Nutr, 1981;34:1617-21.
- Ruderman N, Chisholm D, Pi-Sunyer X, Schneider S. The metabolically obese, normal-weight individual revisited. Diabetes, 1998;47:699-713.
- St-Onge MP, Janssen K, Heymsfield S. Metabolic syndrome in normal-weight Americans. Diabetes Care, 2004;27:2222-28.
- Teixeira TF, Alves RD, Moreira AP, Peluzio M. Main characteristics of metabolically obese normal weight and metabolically healthy obese phenotypes. Nutr Rev, 2015;73:175-90.
- Seaman DR. Body mass index and musculoskeletal pain: is there a connection? Chiro Man Ther, 2013;21:15.
- Seaman DR. The DeFlame Diet: DeFlame Your Diet, Body and Mind. Wilmington: Shadow Panther Press, 2016.
- Seaman DR. The DeFlame Diet to Stop Your Joints, Muscles, and Bones From Rotting. Wilmington: Shadow Panther Press, 2020.
- Punzi L, et al. Post-traumatic arthritis: overview on pathogenic mechanisms and role of inflammation. RMD Open, 2016;2:e000279.
- Gaida JE, et al. Dyslipidemia in Achilles tendinopathy is characteristic of insulin resistance. Med Sci Sports Exer, 2009;41:1194-97.
- Seaman DR, Op Cit (reference #7).