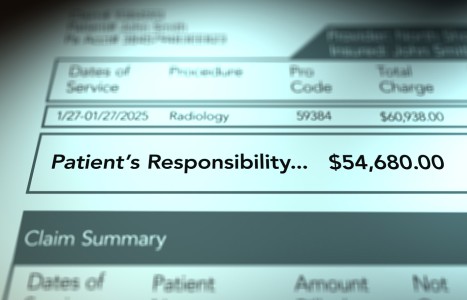
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Accessing the World of Communication Within the Patient
Author's note: The rising tide of both research and public awareness in stress-related issues understandably points our attention to the brain and central nervous system. Accordingly, it is of special interest to the chiropractic profession to be aware of the interconnectedness of the musculoskeletal, immune and hormonal systems, among others. While orthopedically oriented chiropractors have made great strides in addressing the musculoskeletal system, many of their colleagues have at the same time been successfully addressing and utilizing brain, mind, emotional and immunological mind-body connections through a variety of approaches and techniques. Most often, these concepts have been applied to augment the musculoskeletal techniques by specifically addressing the chronic recurring vertebral subluxation. How are all these systems interconnected? The answer might be like the air we breathe, so pervasive it sometimes goes unnoticed. The answer is emotions. All of these non-orthopedic chiropractic techniques eventually interface with the emotions. This series of articles elucidates these vital connections.
Chiropractors are generally known to be excellent communicators with their patients. But what about accessing the complex world of communication that exists within the patient? Herein hangs a tale.
When the first transatlantic telegraph cable was laid in 1858 by Cyrus West Field, little could one have imagined that communication 150 years later would swirl around each and every one of us in a wireless maelstrom of 5G networks, Internets, Facebooks, Instagrams and tweets. The situation is not unlike what has been discovered within our own bodies in the past 100 years.
It turns out that communication is not just a bundle of electrochemical signals leaping from neuron to neuron across a synapse in a unidirectional, linear fashion; rather, a more complex mode of signaling exists, first described by Ishigami, who in 1919 described the reactivation of chronic tuberculosis infection which correlated with periods of severe personal stress.1
Refinements of this more elaborate means of communication were developed by Dunbar in 1943, Alexander in 1960, and Solomon and Moos in 1964.2 Then in the early 1980s, Candace Pert and Michael Ruff emerged into the spotlight with their demonstration that neuropeptides, chemicals secreted by the brain responsible for modulating our moods and behavior, were signaling cancer cells to metastasize to different parts of the body.3
Endocrine, Immune and Nervous System Cross-Talk
All these observations meant that the endocrine, immune and nervous systems were engaged in a cross-talk that burst open the floodgates of our understanding of all the channels of communication that exist within our bodies. Within ourselves, we could now regard ourselves as the keeper of a vast network of multidirectional, interacting signaling systems with an impressive body of research to demonstrate each one.
Our understanding of this network starts with building blocks known as neuropeptides, small proteinaceous molecules with which neurons communicate with each other. They are defined by three principles:4
- Peptide hormones are a class of chemical signals within the endocrine system that include a short chain of amino acids in their molecular structures.
- Secretion of the neuropeptides is a general property of the nervous system.
- The nervous system responds to peptide signals.
The next step is to consider Pert's observation that mutated lung cancer cells bound to antibodies secreted by macrophages, establishing a connection between cancer, the immune system and toxicity in the body, created by such environmental factors as cigarette smoke.3 Consequently, these mutated cancer cells are found to grow rapidly in response to such peptide hormones as bombesin secreted by the brain. This suggests that the same peptides found in the brain are located in the immune system.
Now one could confirm Ishigami's original suspicion that the nervous, endocrine,and immune systems are functionally integrated in what could be called a psychoneuroendocrine network, creating the field of study known as psychoneuroimmunology (PNI)1 and recognizing that mind and body are firmly connected.
Mind-Body and Our Emotions
These mind-body interactions have become recognized as the bedrock of homeostasis, involving the brain and central nervous system, the hypothalamic-pituitary-adrenal (HPA) axis, and the immune system.5 An even deeper understanding of PNI is achieved by observing how the immune system responds to stress; as well as taking a closer look at the various psychological states,6-7 ranging from ecstasy to depression and anxiety.
This multidimensional welding together of the endocrine, immune,and nervous systems affected by emotion has even given rise to a variety of concepts of the nervous system itself – synaptic, receptor-based and meridian. Indeed, what has been called volume transmission involving all three of these models has been described as a widespread mode of intracellular communication that occurs both in the extracellular fluid and in the cerebrospinal fluid of the brain; with signals moving from source to target cells via energy gradients, leading to diffusion and convection.8
Numerous demonstrations of this elegant interconnection of mind and body systems have been reported:
Autonomic nervous system: The latter can be shown to communicate with the lymphoid compartment by means of the release of norepinephrine and acetylcholine from sympathetic and parasympathetic nerves.9
Endocrine effect upon infection: Administering steroid hormones and opioid-based drugs externally can be shown to influence immune function and susceptibility to infections.9
Musculoskeletal conditions: In both humans and animal models, stress is directly associated with both the onset and severity of rheumatoid arthritis.10
Infectious diseases: People under high stress experience much higher infection rates of cold viruses.11
Heart disease: Individuals, especially the elderly, with high sympathetic activity due to stress are at higher risk for cardiac diseases.12
Insulin-dependent diabetes mellitus: Stress-induced increases in glucose may not be metabolized properly, leading to the onset of diabetes.13
Direct effect of estrogens upon innate and adaptive immunity: Dendritic cells are important antigen-presenting cells responsible for the initiation and maintenance of both innate and adaptive immunity. It turns out these cells express estrogen receptors, which permit the steroid hormone estradiol and other ligands binding to that receptor to regulate the homeostasis of bone marrow myeloid and lymphoid progenitors of dendritic cells.
Furthermore, estrogens have demonstrated the ability to influence dendritic cell differentiation. Finally, both agonists and antagonists to estrogen receptor modulate the activation of dendritic cells, as well as the production of inflammatory cytokines.8,14
Endorphin release and spinal manipulation: A randomized clinical trial, yet to be repeated with larger experimental groups, found an approximately 8 percent increase in the level of the mood-enhancing opioid neuropeptide beta-endorphin occurred five minutes after a single rotary manipulation in healthy, asymptomatic men.15
Such was to suggest a connection between the nervous system and endorphins, the latter having been shown elsewhere to be associated with positive mood (emotion) changes.16,17
The Chiropractic Connection
This is where chiropractors enter the picture. It would appear that chiropractic might have an effect upon the patient's emotions as reflected by the foregoing mood (endorphin) changes. But what if the reverse were true – that some means of accessing the patient's moods directly might enhance the effectiveness and longevity of spinal manipulation?
Such was the reasoning of Scott Walker, who clinically verified that there were noticeable improvements for certain chronic conditions when a related stressful event from the patient's past was identified (utilizing memory and associated physiological engagement) while at the same time a specific vertebral sequence was adjusted.
This approach was termed neuro emotional technique (NET), which supported the hypothesis that unresolved stress or emotional pressure could be a factor in sustaining a chronic or recurring condition.18,19
The intention was to break the patterns of an unresolved "physiological" stress response that tended to exacerbate the pain or physical problem in a vicious cycle.20 In so doing, NET is beholden to the principles of the models of BPS and PNI discussed above and in my previous article.
References
- Biondi M, Zannino L. Psychological stress, immune-modulation, susceptibility to infectious diseases in animals and man: a review. Psychother Psychosom, 1997;66:3-26.
- Ader R, Felten D, Cohen N. Interactions between the brain and the immune system. Annual Rev Pharmacol Toxicol, 1990;30:561-602.
- Pert C. The Molecules of Emotion: The Science behind Mind Body Emotion. New York: Scribner, 2003: p. 171.
- Burbach JP. What are neuropeptides? Methods Molec Biol, 2011;789:1-36.
- Ader R, Cohen N, Felten D. Psychoneuroimmunology: interactions between the nervous system and the immune system. Lancet, 2005;345:99-103.
- Rosenberg V. Psychoneuroimmunology: searching for the main deteriorating psychobehavioral factor. Genetic Social Gen Psych Monograph, 1996;122:129-146.
- Morgan. Psychoneuroimmunology, the placebo effect and chiropractic. JMPT, 1998;21(7):484-491.
- Fuxe K, et al. Volume transmission and its different forms in the central nervous system. Clin J Integrative Med, 2013;19(5):323-329.
- Taub DD. Neuroendocrine interactions in the immune system. Cellular Immunol, 2008;252(1-2):1-6.
- Moynihan J, Ader R. Psychoneuroimmunology: animal models of disease. Psychosomatic Med, 1996;58:546-558.
- Schedlowski M, Schmidt M. Stress and the immune system. Naturwissenschaften, 1996;83:214-220.
- Kielcolt-Glaser J, Glaser R. Psychoneuroimmunology and health consequences: data and shared mechanisms. Psychosomatic Med, 1995;57:269-274.
- Surwit RS, Schneider MS, Feinglos MN. Stress and diabetes mellitus. Diabetes Care, 1992;15(10):1413-1422.
- Kovats S, Carreras E. Regulation of dendritic cell differentiation and function by estrogen receptor response after injury. Cellular Immunol, 2008;25291-2):81-90.
- Vernon HT, et al. Spinal manipulation and beta-endorphin: a controlled study of the effect of a spinal manipulation on plasma beta-endorphin levels in normal males. JMPT, 1986;9(2):115-123.
- Markoff RA, Ryan P, Young T. Endorphins and mood changes in long-distance running. Med Sci Sports Exer, 1981;14(1):11-15.
- Dishman RK, O'Connor PJ. Lessons in exercise neurobiology: the case of endorphins. Mental Health Physical Activity, 2009;2(1):4-9.
- Walker S. Neuro Emotional Technique. Seminar folder, Encinitas, Calif., 2006.
- Walker S. Neuro Emotional Xtra Techniques (NEXT). Seminar manual, 2000.
- Monti DA, et al. Muscle test comparisons of congruent and incongruent self-referential statements. Percep Motor Skills, 1999;88:1019-1028.