It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Pain in the Butt and Lateral Thigh: Pt. 2 - A Case Report
Editor's Note: Part 1 of this article appeared in the February 2019 issue.
A recent case history offers the perfect model for this second installment. The patient is a 25-year-old male who works in a tire store and hurt his low back. He has no specific memory of the injury. I am seeing him four months after the injury because he is unable to do full-duty work due to pain.
He describes the pain as primarily in the left SI area. When he points to his pain, it is just below the iliac crest and 2-3 inches lateral to the SI over the tender Maigne points that usually correlate with the T10-11 nerve.
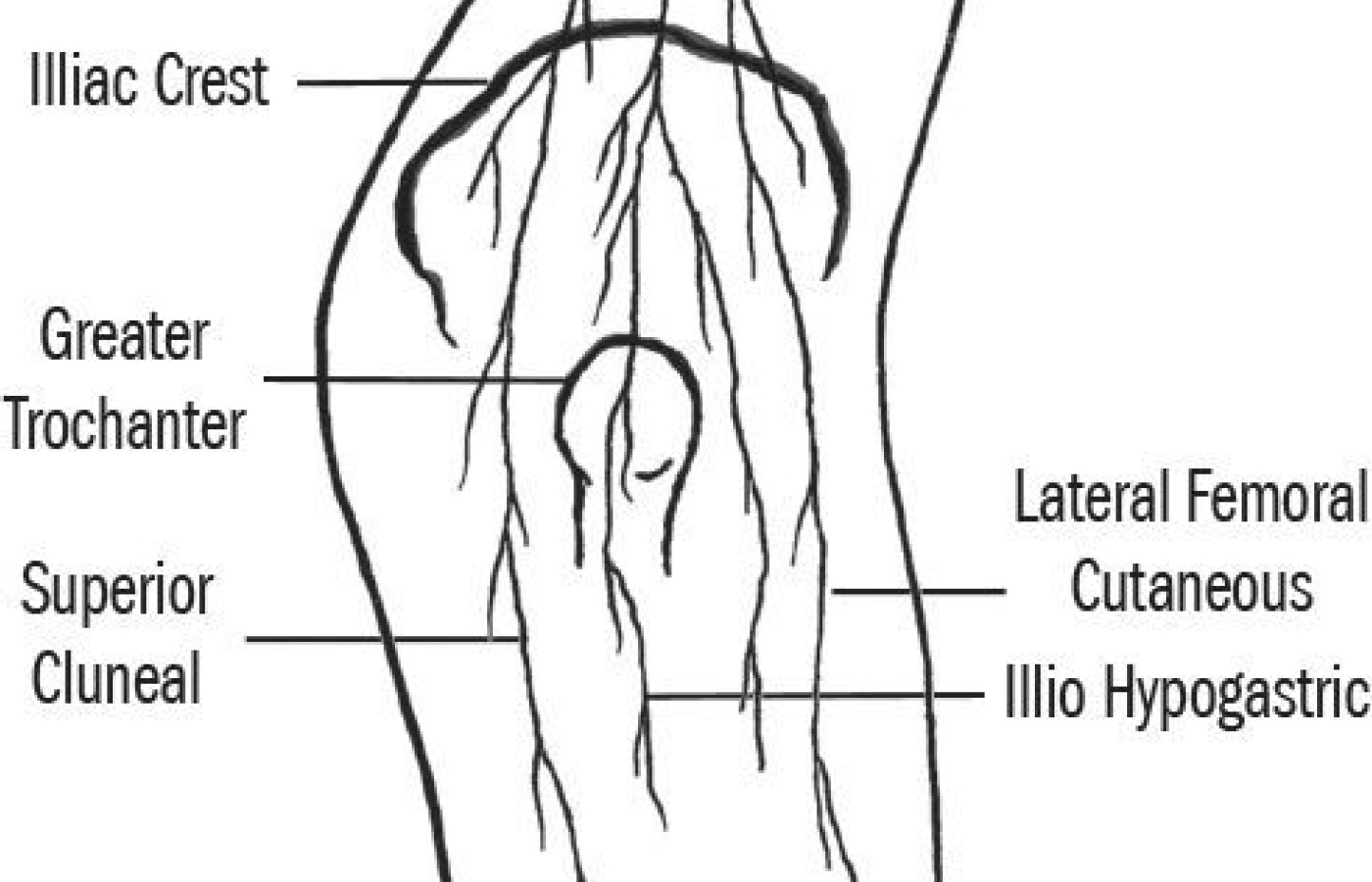
When I palpate just below the iliac crest, he has two main tender points. One is over the T10-11 nerve; the second over the ilio-hypogastric nerve. (For clarification, refer to my thoracolumbar assessment article.)1 The patient displays tenderness and fixation over the TL junction on the left. He mentions that he has some pain in the TL area, but that this started later. He had some vague leg pain initially, but at this point the leg pain is gone.
He is young and fit, strong at the time of injury and is currently doing a "work hardening" type of PT; basically a strong core workout with lifting.
It is possible to reproduce his pain with the combination of extension followed by left posterior rotation. (He had minimal pain on extension and on oblique backward bending. For some reason, this specific motion challenge was more provocative to his involved facet joints.) He also has discomfort on repeated lumbar flexion.
This history and the exam findings make me suspect Maigne syndrome – irritation of cluneal nerves. But the patient could have more than one problem. What's more, I find that if I am more thorough, the patient gets better more quickly. What else was there to search out?
Evaluation / Factors to Consider
- He has no SI indicators. His pelvis is level, legs even length, no tenderness over sacroiliac ligaments and negative SI provocation tests.
- He does have limited left hip internal rotation: 10 degrees on the left side with tenderness over the head of the femur. He is not flexible. The right hip has only about 20 degrees of internal rotation. I interpret this as a unilateral, functional hip impingement.
- He shows both midline lumbar tenderness over the L5 spinous and the typical axial disc-related tender point just lateral to the upper sacrum on the left. These tender points responded to lumbar decompression: hanging from a door with hip hinge. (We tried McKenzie first, which did not change his tenderness.) I suspect an unhappy disc. This is consistent with his pain on lumbar flexion.
- His referring MD, an astute occupational health doctor, noted slight weakness of the left gluteus maximus. After correcting everything else, I tested this with manual muscle testing. The left gluteus maximus is weak, graded 4/5. He has the usual correlate: fixation and tenderness over the upper cervical spine. In this case, his fixation was at left C1. We corrected this with non-thrust, low-force mobilization. His left gluteal strength normalized.
- He displays signs of all three of the most common correctable causes of buttock pain: Maigne syndrome, lumbar discogenic pain and functional hip impingement. He also has an upper cervical fixation creating inhibition of the righting reflexes and extensor inhibition.
Overall Impression & Treatment Plan
- Maigne syndrome, TL joint fixation with cluneal nerve irritation.
- Treatment: TL manipulation and home neuromobilization. Sent him home with suction cups to use the Yank Away Pain (YAP) model to quiet his own nerves at least two times per day.
- Probable discogenic lumbar pain. Pain relief with extension and decompression. He seems to understand the hip hinge model, probably from his experience as a weightlifter. He needs to apply this principle, maintaining lumbar neutral to all of his forward bends and lifts. Core: he is already working on this.
- Left hip dysfunction: Correct with wishbone maneuver and home exercise: side plank plus. Instructed to avoid end-range hip external rotation, which drives the femur further forward.
- Upper cervical dysfunction creating an inhibition of the posterior chain: Correct with manipulation. If this recurs, add specific upper neck exercises.
- Review his exercises to make sure he is not doing flexion exercises, and fine tune his daily motions. I suspect he needs minimal rehab input beyond the specifics outlined above.
The Clinical Takeaway
Damned if you do, damned if you don't (extension vs. flexion): Patients who have both TL / Maigne issues and disc problems are challenging. They can irritate their spine and nerves with extension, secondary to facet joint irritation. They can irritate their disc problem with flexion. They often have, at least initially, a narrow range of comfortable neutral.
What can contribute to lateral hip pain and the tight iliotibial band? When tender points are found on, over or near the greater trochanter and down the IT band, what do you do? Do you release the tight fascia with your IASTM or ART over and over? Do you focus on rehab to the gluteus medius?
I have a hypothesis about another contributor to these pain patterns. The Maigne syndrome nerve irritation of the cluneal complex is a major contributor to lateral hip pain, usually diagnosed as trochanteric bursitis, and tightness / tenderness along the lateral thigh, usually called iliotibial band syndrome. From a neurocentric perspective, both conditions reflect irritation of the sensory nerves [see image] that begin in the thoracolumbar region, run through the iliac crest and then down the lateral thigh. The main joint dysfunctions that contribute to these nerve findings are the facet joints of the TL and a fixated forward hip joint.
Try This on Your Next Patient With Butt Pain and Lateral Thigh Tightness
Begin by palpating below the iliac crest, identifying irritation of the superior cluneal, ilio-hypogastric and/or lateral femoral cutaneous nerves. Then follow the nerve lines into the posterolateral hip. You'll probably find a series of tender points. Keep palpating down the lateral line along the IT band.
Mark all of the tender points. Next, analyze the thoracolumbar fixations and assess hip motion. Treat the fixated, tender TL joints and hip joints with manipulation. Treat the involved nerves with the YAP model, lifting and wiggling the tender nerve points. Teach the patient to do this at home. Reassess your marked lateral tender points. If they are substantially less tender, you've identified another contributing factor to the ITB or trochanteric tenderness.
Reference
- Heller M. "How to Find and Fix TL Nerve Impingements." Dynamic Chiropractic, April 15, 2016.