It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Text Neck: Assess and Adjust
A common presentation in a chiropractic clinical practice is the patient with neck pain and stiffness. Patients usually report limited range of motion on rotation of the head and neck. Some patients say the restriction is pain-limited, while others report just a painless feeling of stiffness.
Onset for an uncomplicated cervical syndrome can be variable and may include activity such as working with the head and neck in flexion for extended periods of time ("text neck") working overhead with the neck in extension and rotation, or "sleeping wrong." For this discussion, we focus on text neck, a term coined by Dean L. Fishman, DC.1
Clinical Consequences
The incidence of text neck has become so ubiquitous that some researchers have begun to call it an epidemic.2-4 One study suggests 79 percent of the young adult population (ages 18-44) use cell phones for most of their waking day, and are therefore vulnerable to repetitive strain injury of the upper back, neck and shoulders.1
Hansraj addresses stresses to the cervical spine resulting from anterior weight-bearing of the head and neck associated with mobile-device use.5 "Forward head posture," notes Hansraj, "increases weight bearing on cervical spine."

The long-term effects can include weak upper back muscles and increased thoracic kyphosis, headache, upper extremity dysesthesia, and pain in the neck, shoulders and upper back. There is also the potential for cervical disc herniation, as well as degenerative joint and degenerative disc disease of the upper spine.
For the chiropractic clinician, the text-neck epidemic can generate a fairly large volume of patients with complaints of neck pain and stiffness. Patients may also present with symptoms in the upper back and shoulders, and it is not unusual for patients to report headache, altered vision, and fatigue. Additionally, long-term consequences of progressive text neck syndrome may cause rounding of the shoulders, thoracic hyperkyphosis, and eventual reduction of respiratory volume.
Assessment Tips
Assessment of the cervical complaint should include history, evaluation of range of motion, static and motion palpation, as well as routine orthopedic and neurological testing. While taking the history, be sure to inquire about the patient's use of mobile devices, especially cell phones and tablets.
Observation and evaluation of postural anomaly – especially anterior position and weight bearing of the head – is an essential part of the assessment of the patient with text neck. Keep in mind that the patient must be viewed from the side to reveal the characteristic anteriority of the head and neck associated with text neck syndrome. Ideally, a plumb line from the external auditory meatus should extend down through the deltoid tubercle, just posterior to the greater trochanter and the lateral malleolus.
For practical purposes, motion and static palpatory findings are a reliable method of assessing an uncomplicated fixation in the cervical spine. The method both determines the optimal level(s) for correction and provides a post-assessment strategy. Assessment should include standard range of motion: right and left cervical rotation, right and left cervical lateral bending, cervical flexion and extension.
Take a few seconds to observe the patient performing the six directions actively before performing passive range of motion. Look for asymmetry and abnormal, "ratchety" motion. The patient may verbally or nonverbally indicate pain-limited motion, so be prepared to ask if they can isolate or pinpoint the source of pain.
Bergman and Peterson suggest testing the involved segment for restricted posterior glide with cervical extension.6 To do so, stand on one side of the seated patient. Support the patient by cupping the forehead with one hand. Use the thumb and index or middle finger on the articular pillars to gently push the neck into extension. Note levels of muscle tension and restricted glide of the inferior articular processes up the inclined plane of the facet joint.
Another way to identify the level of dysfunction is to use the Thompson Technique test for cervical syndrome. Before adjusting the pelvis, lumbar and thoracic spine, the patient typically demonstrates leg-length inequality. Have the patient turn the head and neck to one side first, and observe for change in leg length.
Reproduced with permission from Healthyspines.org.
If there is no response with leg length, repeat the procedure by having the patient turn the head and neck to the opposite side. If the initial short leg becomes even as the patient turns the head and neck, cervical syndrome is indicated.
For example, if the patient turns to the right, causing the legs to become even, the cervical syndrome is on the right side. Palpate for a taut and tender nodule (probably a trigger point)7 at the left lamina pedicle junction of the involved segment.
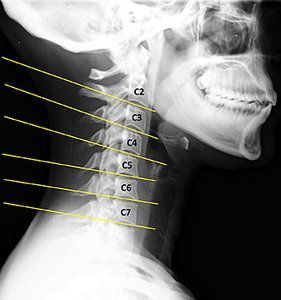
When history and physical findings warrant, cervical X-ray examination may also be part of the assessment. The lateral cervical view in Fig. 1 illustrates some of the findings we would anticipate with chronic text neck. There is evident loss of cervical curve indicated by "military neck or reversed cervical curve." Disc plane lines do not converge to the posterior, but remain parallel or even diverge. Fig. 1 also demonstrates flexion malposition of C4 on C5 (open posterior disc wedge).
Adjusting for Text Neck C2-C6
Correcting the chronic flexion malposition of text neck requires a posterior-to-anterior thrust at fixed segmental level using a table equipped with a drop headpiece. Avoid cervical rotation since that may exacerbate the condition and add to cervical instability.

To set up on an involved cervical vertebra, assume a scissors stance on the side of body rotation at about the level of the patient's humerus. Contact the lamina pedicle junction on the near side with the lateral base of the index finger of the superior hand and use the thumb web to bridge over the back of the neck.
Reach across and contact the lamina pedicle junction on the away side with the lateral base of the index finger of the inferior hand and bridge over the back of the hand with the thumb. Apply a quick, light, toggle-like thrust from posterior to anterior (P-A) through the plane line of the disc.
Remember that the drop mechanism accelerates your manual thrust, so release the thrust as soon as the head piece comes to a sudden stop. Set the headpiece to drop at minimal tension to avoid discomfort to the patient.
Because paraspinal muscles and periarticular soft tissue are likely to be distressed, warn the patient that the adjustment could cause transient irritation. Also, post-checks immediately following the adjustment may yield little useful information. Assessment of the outcome of care is best conducted with a follow-up visit.
Editor's Note: This is article #1 in a series in which the authors address the clinical consequences of electronic device use.
References
- Neupane S, et al. Text neck syndrome – systematic review. IJIR, 2017;3(7):141.
- Vate-U-Lan P. Text Neck Epidemic: A Growing Problem for Smartphone Users in Thailand. The Twelfth International Conference on eLearning for Knowledge-Based Society, Dec. 11-12, 2015, Thailand.
- Burns K. "Text Neck: The Health Epidemic of the Tech Era." American Posture Institute; posted July 4, 2016, in Lifestyle, Posture, Tech Neck.
- Bever L. "'Text Neck' Is Becoming an 'Epidemic' and Could Wreck Your Spine." The Washington Post, Nov. 20,2014.
- Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int, 2014;25:277-9.
- Bergmann TF, Peterson DH. Chiropractic Technique: Principles and Procedures, 3rd Edition. St. Louis: Elsevier-Mosby, 2011.
- Fernández-de-las-Peñas, et al. Myofascial trigger points in subjects presenting with mechanical neck pain: a blinded, controlled study. Manual Therapy, 2007;12,29-33.



