It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
An Overlooked Tool for Musculoskeletal Injuries
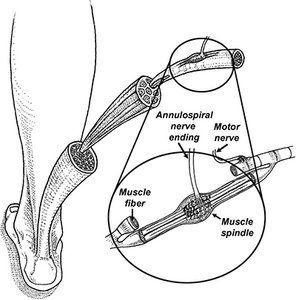
Initially discovered in the 1960s by Eklund and Hagbarth,1 a surprising body of research has shown that placing small vibrating motors over the belly of a muscle can produce presynaptic inhibition of the muscle's spindles, which can reduce muscle tone by as much as 50 percent.2 (Fig. 1)
Lee, et al.,3 suggest muscle vibration reduces tone by changing the intracortical inhibitory circuit. Best results are achieved with motors that oscillate at 60 cps with 0.4 mm displacements. The sharp reduction in muscle tone associated with focal vibration provides a useful clinical tool for managing a range of musculoskeletal conditions.
A Novel Use for Muscle Vibration
While early research on focal vibration focused on treating muscle spasticity, more recently, Kurt Claeys and his colleagues from Belgium4-5 came up with a novel diagnostic use for muscle vibration. These authors published a series of papers showing that while we are standing with eyes closed, the muscle spindles in our calves and core muscles share information, allowing us to balance properly.
Apparently, the calf muscles send information to the central nervous system regarding forward / backward sway while core proprioceptors give information regarding the position of the torso relative to the pelvis. The shared information regarding position sense is vital for injury-free activity, since muscle spindle input tells your central nervous system exactly where you are in space and what speed your joints and muscles are accelerating / decelerating.
Of course, this information is also vital for injury prevention, as it allows for the smooth, controlled motion necessary to participate in most daily activities. Perfectly functioning proprioceptors are especially important in preventing sports-related injuries.
In their clever studies, the Belgian researchers decided to use muscle vibration to evaluate the sensitivity of an individual's core proprioceptors. Claeys, et al.,4 placed vibrating motors on the soleus muscle while subjects stood on force platforms with their eyes closed. When these motors were turned on, the sudden vibration caused presynaptic inhibition of the muscle spindles (specifically the annulospiral nerve endings), producing the false sensation that the soleus muscle was lengthening.

In subjects with perfectly functioning core proprioceptors, the core muscles ignored the faulty information from the vibrating soleus muscles, and the subjects easily managed to balance with eyes closed. Conversely, subjects with poor core proprioception immediately shifted their entire body back to counter the illusion that they were falling forward. The degree of posterior sway was readily measured with a laser centimeter scanner (Fig. 2). This simple test takes less than 20 seconds to perform and provides information regarding core proprioception that until recently, was impossible to obtain.
To determine if muscle vibration can distinguish between asymptomatic and chronic low back pain patients, Claeys, et al.,4 performed the 20-second muscle vibration test on 106 nonspecific low back pain patients and 50 healthy controls. The researchers confirmed that LBP patients had significantly greater backward sway when their calves were vibrated, which the authors relate to reduced "lumbosacral proprioceptive." The authors theorize that the LBP patients were unable to process proprioceptive signals from their low back muscles and were forced to become overreliant on calf proprioceptors.
This study is fascinating in part because so few clinical tests can distinguish LBP patients from non-LBP patients; e.g., arthritis and herniated discs are considered normal variants in individuals with low back pain.
In a follow-up study, Claeys, et al.,5 again performed the 20-second vibration test on more than 100 asymptomatic subjects. In addition to evaluating vibration-induced sway, the authors also evaluated spinal posture along with various psychosocial behaviors known to correlate with the of future development of low back pain; e.g., fear avoidance behavior.
The subjects were followed for two years, and while posture and fear avoidance behavior in no way predicted the development of low back pain during that period, individuals who swayed excessively when their calf muscles were vibrated were almost four times more likely to hurt their backs over the two-year follow-up period. As with differentiating low back from non-low back pain patients, this finding is significant since so few factors predict future injury.
The Role of the Diaphragm
Because increased postural sway following calf vibration predicts future back injuries in asymptomatic populations, the next phase of vibration research focused on identifying which factors result in impaired core proprioception and then evaluating which, if any, interventions can improve core proprioception.
To that end, Lotta Janssens, et al.,6 showed that a weak diaphragm can impair core proprioception by decreasing sensitivity of spindles located in the low back muscles. Apparently, because oxygen is necessary for our survival, the central nervous system prioritizes the delivery of blood to the diaphragm over other skeletal muscles. When the diaphragm fatigues with exercise, the central nervous system deliberately decreases blood flow to spinal and peripheral muscles in order to shunt as much blood as possible to the diaphragm.

If an individual's diaphragm is weak, it prematurely fatigues and blood is redirected away from peripheral muscles to enhance diaphragmatic circulation. Several studies have shown significant reductions in blood flow to the erector spinae and lower extremity muscles when the diaphragm is deliberately exhausted.7-8
Clinical Takeaway
Over the past year, I've had patients with excessive vibration-induced posterior sway perform a series of different exercises, including diaphragm and various lower extremity exercises. I've also used hip mobilization, spinal manipulation and deep-tissue massage of the erector spinae musculature to see what, if anything, can improve core proprioception.
While spinal mobilization and deep-tissue massage will occasionally increase core proprioception, without doubt the most significant improvements in posterior sway occur when performing exercises to increase endurance to the lumbar paraspinal muscles.
My favorite exercises for restoring low back proprioception are summarized in figure 3. It is not uncommon to have full restoration of core proprioception within the first eight weeks of performing these exercises. Of course, a weak diaphragm should always be strengthened and a hypomobile spine and/or hips should always be mobilized.
References
- Eklund G, Hagbarth K. Normal variability of tonic vibration reflexes in man. Exp. Neurol,1966;16:80-92.
- Voerman G, Gregoric M, Hermens H. Neurophysiological methods for the assessment of spasticity: the Hoffmann reflex, the tendon reflex, and the stretch reflex. Disabil Rehabil, 2005;27:33-68.
- Lee G, Cho Y, Beom J, et al. Evaluating the differential electrophysiological effects of the focal vibrator on the tendon and muscle belly in healthy people. Ann Rehabil Med, 2014 Aug;38(4):494-505.
- Claeys K, Brumagne S, Dankaerts W, et al. Decreased variability in postural control strategies in young people with non-specific low back pain is associated with altered proprioceptive reweighting. Eur J Appl Physiol, 2011;111:115-123.
- Claeys K, Dankaerts W, Janssens L, et al. Young individuals with a more ankle-steered proprioceptive control strategy may develop mild nonspecific low back pain. J Electromyogr Kinesiol, 2015;25(2):329–338.
- Janssens L, Pijnenburg M, Claeys K, et al. Postural strategy and back muscle oxygenation during inspiratory muscle loading. Med Sci Sport Exerc, 2013;45(7):1355-62.
- Harms C, Babcock M, McClaran S, et al. Respiratory muscle work compromises leg blood flow during maximal exercise. J Appl Physiol. 1997;82:1573-1583.
- Borghi-Silva A, Oliveira C, Carrascosa C, et al. A respiratory muscle unloading improves leg muscle oxygenation during exercise in patients with COPD. Thorax, 2008;63:910-915.



