It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Improving Ankle Mobility to Improve Overall Movement
What is the underlying cause of joint or movement restriction? Absent trauma, the brain will put a "governor" on the body to restrict movement when the brain feels movement will put the body at risk of injury. This is akin to a golf course putting a "governor" on golf carts. Golf courses do not want golf carts zipping around the course due to risk of injury for golfers who would drive at unsafe speeds.
Mobility vs. Stability
The body's "governors" are typically found in areas of the body meant to be mobile. As clinicians, we see these joints and areas as requiring mobility (manipulation, stretching, etc.). For example, when you ask a patient to touch their toes and they cannot, how do we know if the problem is the ankle joint, hamstring, hips, lower back or thoracic spine? All these areas contribute to the movement of toe touch. Typically, our patients will say something along the lines of, "I've always been tight in my hamstrings; that's why I can't touch my toes." Could it be the brain tightens the hamstrings to prevent the toe touch because the core is not stable enough to tolerate the forward bending? Yes, at least some of the time.
All joints require a balance between being mobile and stable. Although the shoulder joint has the most degrees of freedom, without stability built in, the body wouldn't be able to control all that mobility without risk of injury. How do we know if a joint or region is supposed to be primarily mobile or stable?
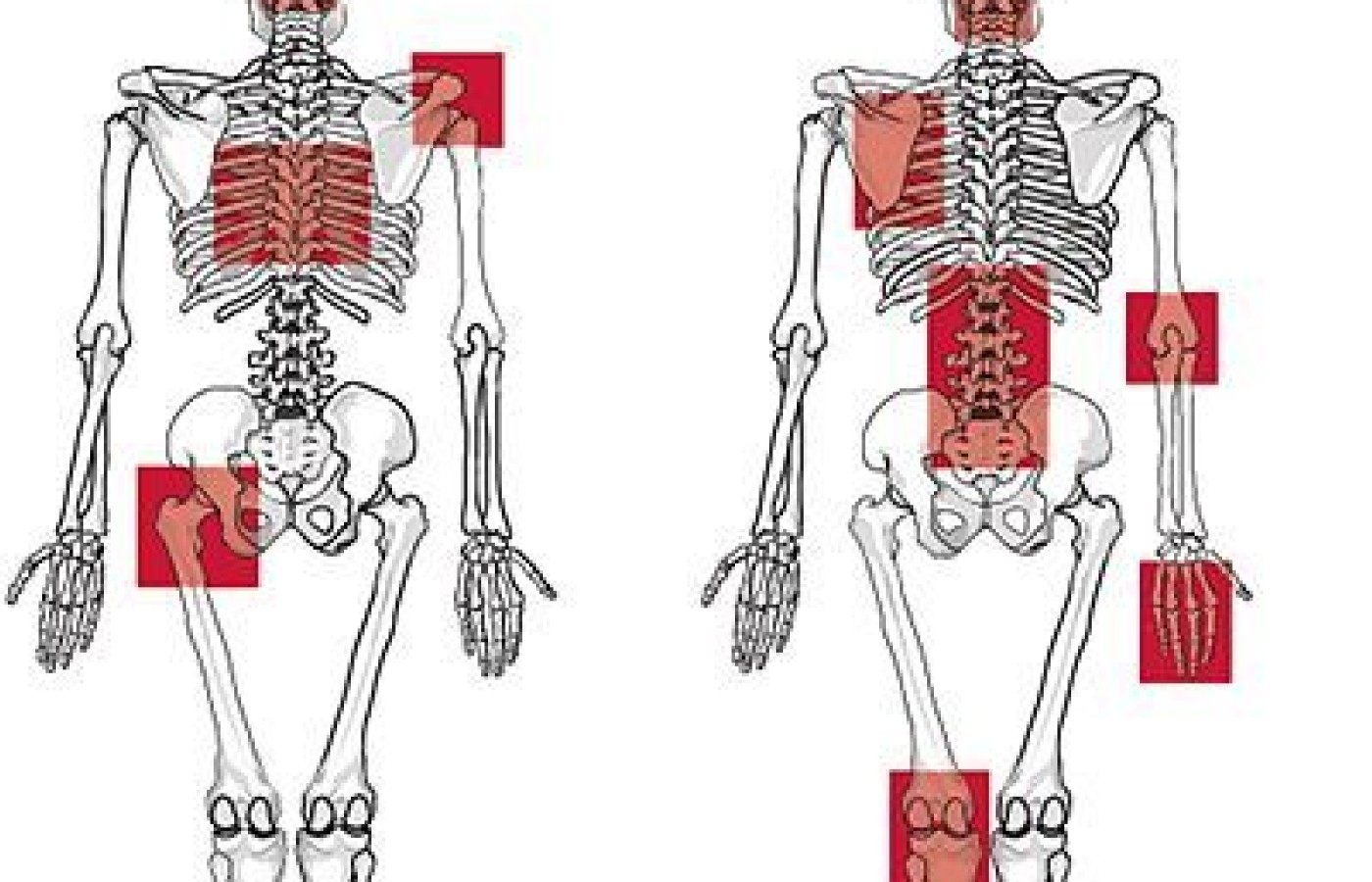
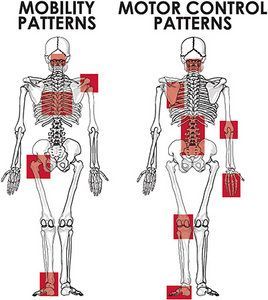
Physical therapist Gray Cook and strength coach Mike Boyle came out with a joint-by-joint approach to the human body. They list both mobility areas and stability areas. I added a few more to this list that are chiropractic specific (big toe, foot, lower / upper cervical). See Figure 1 for mobility areas and Figure 2 for stability / motor control areas.
- Big toe: mobility
- Foot / arch: stability
- Ankle: mobility
- Knee: stability
- Hip: mobility
- Lumbar spine: stability
- Thoracic spine: mobility
- Scapula: stability
- Glenohumeral (shoulder): mobility
- Lower cervical: stability
- Upper cervical: mobility

Notice the regions alternate between mobility and stability. The reason for alternating mobility / stability patters is so forces distribute throughout the body without putting excessive trauma in one area. For example, if the hip is not mobile enough, the forces will transmit to the areas above and below (lower back / knee).
Stability can also be termed motor control because what we really need is better communication between the brain and the stabilizing system of the joint, not necessarily increased hypertrophy of the muscles. The stabilizing system is composed of active (muscle), passive (joint) and neurologic (brain and nerves).
Screening Movement
Begin by asking the patient what activities aggravate the condition. Is it knee pain with a squat? If so, I would watch the patient do an air (unloaded) squat. Does that replicate the pain? If so, how good is the squatting movement? If the movement doesn't pass the standards for quality movement, it is time to assess why the movement is poor.
Is there a lack of mobility in a joint that requires good mobility If there is a lack of mobility in a joint, is it because of a joint problem, a soft-tissue issue or lack of motor control? If there is plenty of mobility in each joint when you isolate it, the problem is how they play together in a synchronized fashion (motor control).

Houston, We Have a Problem
Once we know there is a problem, we have to figure out the best way to approach the solution. Removing the stress from the system and isolating each joint can reveal areas that need to be addressed further. The stress in this case is gravity from being in an upright position.
Take the patient from a loaded position, in which gravity is influencing movement, to a seated or lying position. If the joint appears to not be moving well in weight-bearing, but in non-weight-bearing, there is plenty of movement, we know it is a motor control issue. Soft-tissue or joint problems don't disappear once taken out of weight-bearing, and motor control problems will be inconsistent between movements and positions.

In the case of the ankle, we may have a squat that is not optimal. In Figure 3, the athlete is unable meet the criteria of getting her thigh parallel (or below parallel) to the ground. The problem is either a joint issue (big toe, ankle, knee or hip) or the brain is putting the governor on the movement.
So, how do we know which? In the beginning, I would utilize a goniometer (The iPhone has great applications for digital goniometers) and measure the joints that require mobility in a non-weight-bearing posture. In the case of the ankle, dorsiflexion should be at least 22 degrees. If we don't have that amount of mobility in non-weight-bearing, we can manipulate the ankle joint and work the soft tissue above and below the joint with soft-tissue manipulation using instruments or our hands.
Home-Care Suggestions
Most important are the exercises we give our patients for home care. True soft-tissue extensibility problems require daily mobilization. Using a myofascial ball in the arch of the foot and a foam roller in the calf helps the soft tissue. (See Figure 4 and Figure 5.)

Figure 6 demonstrates using a 2-inch gym band on the distal aspect of the tibia while going through knee bends. This helps improve range of motion by pulling the tibia posterior. Have the patient perform 20 repetitions after the foam rolling and myofascial ball work described below.
If the tissue and joint work described above improves the range of motion, but restrictions return shortly after (30 minutes to 24 hours), consider the restriction in motion a motor control problem that has been there too long. Resistance exercises will need to be added to this regimen to get the new range of motion to last. I recommend arch exercises and eccentric (lengthening) loading of the back of the lower leg.
Using a movement screen helps to identify areas within the kinetic chain that are not performing well. Breaking down the patient's movement into the pieces helps differentiate areas of joint restriction, soft-tissue extensibility issues or motor control problems. Treat normally as you would in the clinic, but give the patient activities to do at home to help speed up the recovery process.