Some doctors thrive in a personality-based clinic and have a loyal following no matter what services or equipment they offer, but for most chiropractic offices who are trying to grow and expand, new equipment purchases help us stay relevant and continue to service our client base in the best, most up-to-date manner possible. So, regarding equipment purchasing: should you lease, get a bank loan, or pay cash?
Flexion-Intolerant Lower Back Pain (Pt. 3): Mobilization & Soft-Tissue Treatment
Editor's note: Part 1 of this article appeared in the Jan. 15, 2014 issue; part 2 ran in the March 1 issue.
What is the biggest challenge to the chiropractor in treating discogenic pain? You have to completely reframe the purpose of your manipulation. It is rarely about unlocking a stuck segment at the disc involvement level; it is not about putting a joint back in alignment. We attempt to follow the "joint-by-joint" model as applied to manipulation. That means the key places to adjust are likely to be above and below the painful lumbar disc. The odds are that the lower lumbar segments tend toward hypermobility, rather than fixation. Pain will inhibit the deep spinal stabilizers, allowing slope or excessive uncontrolled movement around the affected disc.
1. Assess and Unlock the Thoracolumbar Junction
One obvious place to look for fixation is the upper lumbar and lower thoracic segments (the TL junction). As the TL gets stiffer, the lower lumbars have to move more. When you check the lower thoracic and upper lumbar, it is useful to assess whether this fixation has caused or contributed to impingement of the superior cluneal nerves.1

We used to think this was just one more significant piece for apparent lower lumbar pain. Since being exposed to Lyftogh's work, we are further convinced that this area is critical for any lower back pain.2 Lyftogh has an impressive case-series article on treating chronic lower back pain by decreasing inflammation in the superior and middle cluneal nerves with dextrose injections.
Here is a brief outline of how to further assess this area. Maigne and Lyftogh have noted two points just below the iliac crest. The more medial is 7-8 cm lateral to midline, and can represent the nerves that exit from L1-2-3. The other is about 11 cm lateral, and can represent the T10-T12 segments. These points are where the nerve goes over the iliac crest, and where the nerves go through either osseofibrous tunnels or through the posterior fascia.
They are classic tunnel syndrome tender points. If these points are tender and swollen, the nerve is irritated. You can follow a straight line back to the spinal fixation, and continue that line down below the iliac crest through the glutes toward the greater trochanter. You will likely find additional tender points.
The first thing to do is to find the fixation and adjust it. We find it particularly useful to check the sides of the spinous process, both for tenderness and for a lack of lateral bending. Recheck the tender points as indicators of whether your adjustment was effective. These tender points are their own pain generators, and need local treatment as well. Local treatment can be dry needling, e-stim, laser or LED light.

Although we have no definitive evidence of this, our impression is that irritated nerves respond quite consistently to light therapy. Counterstrain-type approaches, approximating the tissue, also seem to work well. (We will talk more about this peripheral neurogenic inflammation in our next article.)
2. Check and Correct Hip Motion; Release the Psoas
The other key is the hip joints, which allow significant motion when they function well. When the hip gets stiff, it requires the SI and lumbar spine to move more to allow any twisting or bending. The hips typically lose flexion and internal rotation. If the hips cannot flex, then the lumbar spine will excessively flex – the enemy of the flexion-intolerant back patient. When the hips lack internal rotation, the lumbar spine will have to increase rotation, again getting the disc in trouble.
To quote Mike Boyle:3 "The biggest mistake I believe we have made in training over the last ten years is engaging in an active attempt to increase the static and active ROM of an area that obviously craves stability. I believe that most if not all of the many rotary exercises done for the lumbar spine were misdirected."
How else can we prevent increased lumbar rotation and flexion? Get the joints (the hips) that are supposed to flex and rotate more mobile via mobilization. Get the hips moving if they are stuck. The wishbone maneuver is great for this,4 but you can use whatever method you like. Always, assess, treat and reassess. Does the hip move better when you are done? Is the head of the femur less tender?
Don't forget the psoas. This muscle is pivotal in any dysfunction of the thoracolumbar area, the hips and any lumbar problem. Remember that the psoas is directly in front of the lumbar vertebral bodies and discs. Releasing the deep psoas at the level of the problem (or wherever you find the restriction) can really make a difference.
Be specific; the psoas has segmental innervation. The hot spot will often be most prominent on one side and at one or two levels.
3. Assess and Treat the Sacroiliac Joint
We mentioned in our previous article that the presentation of these patients is often mixed, with obvious SI misalignment. The SI may be either fixated or hypermobile, or both simultaneously. Treat the SI, but don't have the illusion that it is the whole problem.

We recommend against side-posture, rotational, high-velocity adjusting when adjusting the SI. There are many ways to realign and mobilize the SI without thrusting. If you suspect a disc, avoid high-velocity rotation to avoid putting further stress on the disc – first do no harm. The SI is clearly part of the lumbopelvic area that tends to get too mobile in the joint-by-joint model, so only treat fixated components. Be gentle.
One important specific fixation of the SI is a common pattern on the sacral side of the SI joint. The muscle energy model calls this a backward or posterior torsion.5 On the stuck side, the sacral base will not be able to nutate / extend. Extension is often the best self-therapy for the disc, but if one side is stuck, unable to extend, the patient cannot effectively extend. We are describing for you a newer method of correcting this thanks to Lucy Whyte Ferguson, DC.6
[Editor's note: Dr. Heller has updated this in his newest video class at HealthPath Education.7]
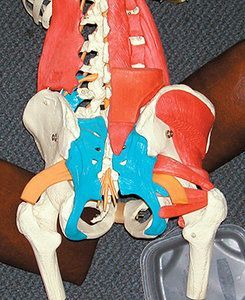
Correction of sacral posterior torsion is pictured below. It's simple. Stand on the involved stuck side. Contact the prominent (posteriorly rotated) side of the sacral base with your hypothenar contact. Lift the patient's bent lower leg to about 30 degrees. Have them isometrically push their lower leg toward the table as you resist. They are attempting to straighten the leg.
As they do this contraction, push the sacral base posterior to anterior. Do this for 5-10 seconds and repeat two more times. You can fine tune on the second and third reps by abducting the patient's leg to about 20 degrees and rotating the lower leg outward toward you about 20 degrees (which internally rotates the hip). Same contract action: Patient pushes down while you push the sacral base P to A. This is an eccentric correction, a little variation on muscle energy, which is contract/relax.
4. Decompress the Disc
Are there useful mobilizations that can be done at the level of the probable disc problem? This area is likely to be hypermobile and unstable. But within the hypermobile area, there are likely to be either stuck joints or compressed areas.
When the interspinous interspace is tender, specific in-office decompression can be helpful, whether you use a flexion-distraction table, a vertebral distraction pump tool or manual pumping of the disc. We've used specific decompression during our whole careers, but we see it differently today. Our default technique here is SOT category three blocking, done prone, while simultaneously pumping the disc open, either manually or with a vertebral distraction pump.8
Sometimes, more specific decompression seems to really do something above and beyond more general decompression. [Dr. Heller wrote about a possible model for how flexion distraction may work, based on Brian Mulligan's model.9] The idea is that when the lower lumbar facet is stuck closed, resisting flexion, it impacts function of the whole three-joint complex, including the disc.
When we are doing a variation of specific decompression,we really pay attention to our specific line of drive. Sometimes it is about just axial decompression; sometimes you need to use a different line of drive. As always, use an assess-treat-reassess model. In this case, a useful indicator is decreased tenderness in the interspinous spaces or tenderness over the sides of the lower lumbar spinous processes. Another useful test is changes in the ease of bending into flexion. Whatever form of decompression you use in-office, the patient needs to reinforce this with McKenzie extension or decompression exercises.
The patient may have fixations, joint dysfunctions at the level of the disc, or just above or below. It is appropriate to correct these. Again, use caution, stick with low force and don't take the spine into end-range flexion and/or rotation.
What else? When the patient is acute and in muscle spasm, you can sometimes break the cycle through some form of soft-tissue release. Targets include the psoas, as mentioned previously, and the quadratus lumborus. Again, search above and below as well. Lower thoracic paraspinal muscles can get very rigid. The glutes and deep external rotators often have significant tender points.
One warning: If you are strictly treating the patient while they lie prone, they may get some relief and some relaxation, and then have a sudden recurrence of severe spasm as they begin to bear weight once again. Anticipate this possibility by showing the patient simple abdominal bracing prior to getting them to move from the table.
First, ask them to be absolutely relaxed while you gently rock their hips back and forth on the table. Then ask them to do the opposite – "Don't let me move you" – while you perform the same hip / pelvis rocking motion. Palpate the lateral abs and tell the patient to keep that area braced while moving off the table.
This is a good time to encourage them to use this strategy at home with transitional movement to avoid pain. If this spasm still occurs, note it and limit prone time to 5 minutes or less. If you have the patient prone for a while, take a 30 second break, and have them practice bracing, do McKenzie extension, and/or get up on all fours and do gentle pelvic tilting.
If the patient gets up from your table and is stuck, bent over in spasm, don't just stand there. Help with your hands. Have the patient stand facing a wall, with their hands on the wall. Gently and firmly guide and push them out of their flexion posture into further extension. Think of this as a variant on the McKenzie model, done standing, with doctor help. The patient will be afraid of this, as they are in acute spasm and pain, but it works. You can also do this prone if the patient is unable to stand.
The disc can be either acutely or chronically inflamed in the flexion-intolerant patient. When the nucleus is leaking nuclear material into the annulus, this can set off ongoing severe inflammation. We have outlined strategies to keep the person from continually re-irritating the disc with poor movement. You may find that nutraceutical or pharmaceutical anti-inflammatories are helpful here. When the acute flared-disc patient is not responding to our conservative care within two weeks, we typically send them out for either oral steroids or an epidural injection.
Conclusions (and Don't Neglect Self-Care)
We deliberately left the mobilization and soft-tissue part of treatment for the flexion-intolerant low back to this last article of the series. We firmly believe, with good evidence, that you have to use self-care and rehab to help these patients. Always start by establishing the hip hinge and starting to change their aberrant movement pattern.
Our care can help flexion-intolerant and disc-pain patients. In our opinion, our care, done right, is superior to the patient getting repeated steroid injections over and over. Our care, done right, can prevent unnecessary fusion surgeries. Yes, we should be treating lumbar disc patients.
We believe the best outcomes occur when you are broad in your approach, including appropriate rehab. It certainly helps to have a cooperative attitude in working with the rest of the medical team with these patients.
References / Further Reading
- Heller M. "Thoracolumbar Junction or Superior Cluneal Nerve Entrapment Syndrome; A Hidden Source of Low Back & Pelvic Pain." Dynamic Chiropractic, Nov. 4, 2011.
- Lyftogh J. Prolotherapy for recalcitrant lumbago. Australasian Musculoskel Med, May 2008.
- Boyle M. A Joint by Joint Approach to Training,
- Heller M. "The Hip Joint, Myofascial and Joint Patterns." Dynamic Chiropractic, May 7, 2007.
- Heller M. "The Sacral Side of the SI Joint: Correcting Anterior and Posterior Torsions." Dynamic Chiropractic, Dec. 16, 2010.
- Conversations on technique with Lucy Whyte Ferguson.
- Heller M. Online video course: Part B: The Joint by Joint Approach - Pelvis and Hips. Health Path Education
- Heller M. "Correction of Discogenic Pain and Midline Tenderness." Dynamic Chiropractic, Oct 6, 2003.
- Heller M. "More Low Back Explorations: Disc vs. Facet vs. Sacroiliac." Dynamic Chiropractic, July 29, 2012.



