It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Managing Hallux Hypomobility Disorders (Part 2)
Editor's note: This two-part article on hallux joint dysfunction and chiropractic treatment strategies is the initial installment in an ongoing series on chiropractic management of lower extremity disorders.
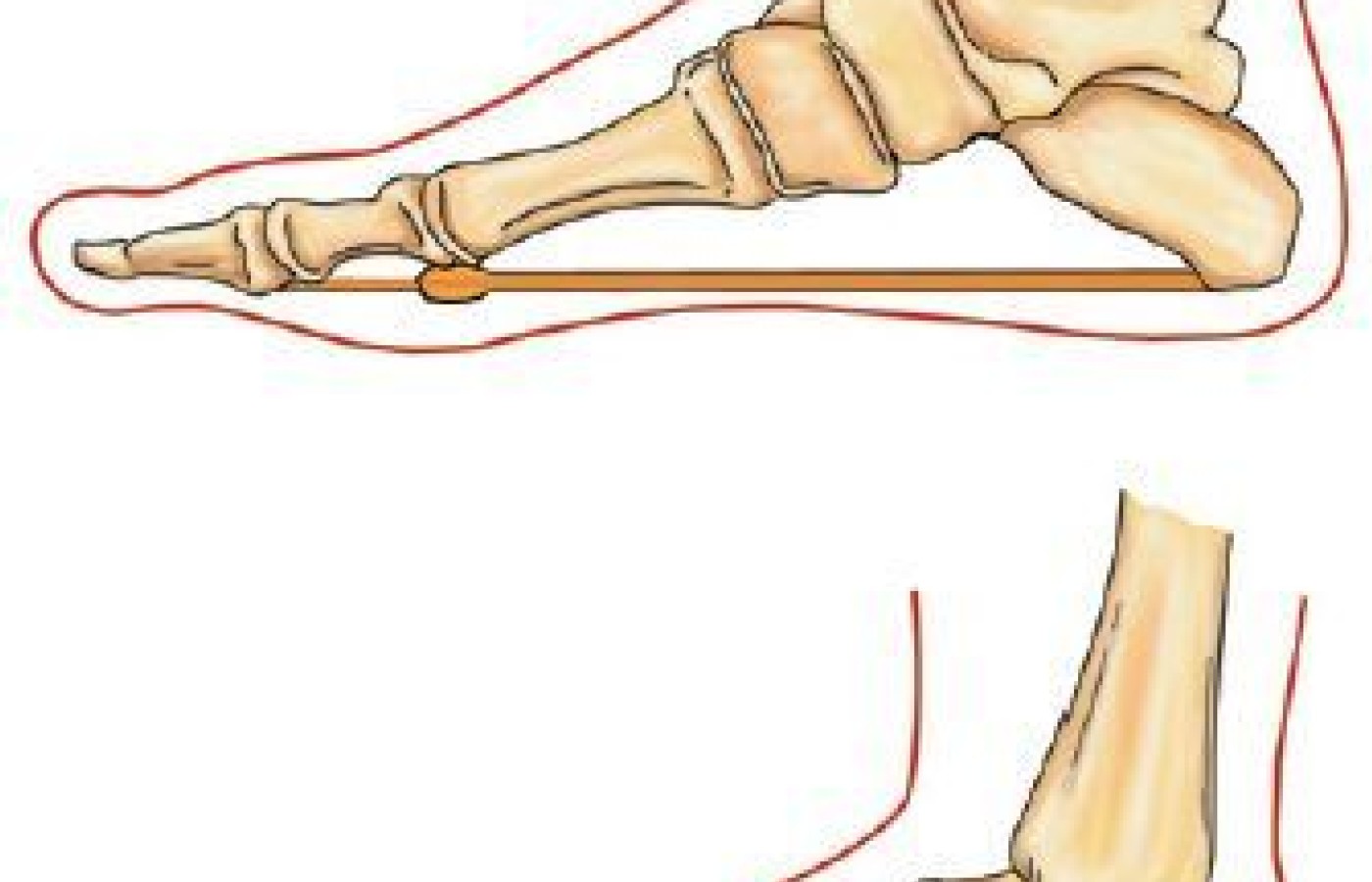
In part one of this series we discussed the unique properties and significance of the first toe in the propulsive phase of gait. In particular, we discussed the importance of the first metatarsophalangeal joint (MPJ). The MPJ uses the windlass effect to raise the arch and stiffen the foot during dorsiflexion of the hallux. (Figure 1) This stiffness increases the efficiency of the propulsion portion of the gait cycle. To be efficient in creating stiffness, the hallux should be able to dorsiflex at least 65 degrees. The normal passive range of motion of the MPJ is 50-100 degrees.
We also discussed some maladies that impede hallux dorsiflexion. These conditions include hallux limitus, hallux rigidus, and turf toe. Hallux limitus is when the passive dorsiflexion of the first MPJ is 60 degrees or less, and hallux rigidus is when first MPJ dorsiflexion is 30 degrees or less. Conservative management of hallux hypomobility will involve one of two treatment paths.
Three Paths of Allopathic Care, Two Paths of Conservative Treatment
The three treatment options available for allopathic care are essentially drugs, injections or surgery. These all have a place in care, but only after more conservative care has failed, and the patient's pain and dysfunction are refractory.
There are two basic conservative options for treating hallux hypomobility: (1) support the MPJ with an orthotic; (2) increase the motion of the MPJ with adjustments and exercise. Both of these treatment options have merit under the proper circumstances and are detrimental under the wrong circumstances. Many patients whose hallux conditions have not progressed too far respond to combining these conservative treatments.
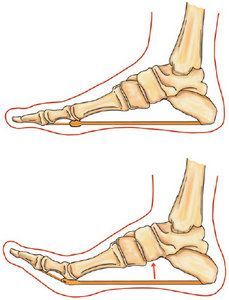
In severe cases of hallux rigidus, the pain and degeneration are so advanced that adjustments and motion-enhancing stretches would be provocative and should be avoided. In these cases, an orthotic or a rocker-bottom shoe can provide pain relief and an artificial stiffness of the foot. While natural movement patterns are always preferred to artificial, there are times that artificial supports will minimize the effects of severe degeneration and should be considered.
There are many types of orthotics that may be used and an incredible divergence of opinion exists on which type of orthotic is preferred. One that is popular with our hospital's orthotic department is a carbon-fiber orthotic, which limits motion of the MPJ while providing stiffness to the medial arch of the foot. This stiffness enhances propulsion, but may place biomechanical burdens upon other joints of the lower extremity, pelvis and spine.
Determining the Course of Care: Adjustment, Support or Both?
This is a relatively easy question to answer. Patients who feel better with adjustments should start with adjustments; patients whose condition is aggravated by increased motion should be treated with an orthotic. Patients who tolerate motion well, but do not progress, may try a combination of manual care and orthotics. Patients with the following criteria may be better suited for support, rather than adjustments:
- Ankylosis of the MPJ
- Advanced degenerative joint disease
- Exostosis, which limits dorsiflexion of the MPJ
- Sustained pain with normal activities, passive joint motion, joint glides, and adjustments
- A reduction in pain with support from stiff soles, rocker-bottom shoes, athletic taping or a stiff orthotic
Essentially, those who feel better with support should get support; those who feel better with adjustments should get adjustments. Those who fail conservative care may try, in ascending order: oral medication, joint injections and surgical intervention.
Examination Prior to Performing Manual Treatment
In addition to a standardized examination of the patient that would include history, vital signs, systemic review and examination, and an orthopedic and neurologic examination, there should be a dedicated evaluation of the foot. The foot examination should address vascular health: pedal pulses, capillary refill time and visual appearance.
Motion palpation of the hallux is performed by grasping and stabilizing the first metatarsal with one hand and grasping the proximal first phalynx with the other hand. Test the accessory motion of this joint in A-P glide, medial-to-lateral glide, eversion-inversion, and long-axis distraction. Observe for reduced joint motion, fusion, pain, instability or deformation. If uncertain about whether the accessory joint motion is normal or not, motion palpate the other hallux MPJ for comparison.
Absent findings of rheumatological, neurological, endocrinological or vascular diseases, deformation such as hallux valgus, and orthopedic damage such as fractures or soft-tissue damage, manual treatment can be attempted.
Adjusting the Hallux
There are several ways to adjust the hallux. The least traumatic way to increase motion in a hypomobile hallux joint is with low-velocity mobilizations or joint glides. The doctor faces the medial portion of the foot to be treated and with the proximal hand grasps and stabilizes the first metatarsal, and with the distal hand grasps the first proximal phalynx. Then the phalynx is put through these joint glides: anterior-posterior, medial-to-lateral, eversion-inversion, and long-axis distraction. The glides should be smooth and controlled mobilizations of the joint.

If joint glides are well-tolerated, the doctor may progress to an impulse. Motion palpate the various aspects of hallux MPJ accessory motion. If a fixation is perceived, give a high-velocity, low-amplitude impulse through the fixation.
Adjusting the hallux with a "pistol grip." The doctor grasps the MPJ of the hallux between the index and middle finger of the lateral hand. The medial hand supports the grasping hand and can provide a gentle medial-to-lateral pressure. (Figure 2) The doctor distracts the joint to tension and then provides a quick, long-axis distracting impulse.
There are many ways to treat the hallux, and we are only introducing a few in this article. These techniques are best observed in our video instruction.
Soft-Tissue Mobilization and Self-Mobilization

In addition to articular restrictions, myofascial restrictions of the flexor tendons, plantar fascia, and joint capsule may restrict motion of the hallux. We recommend using instrument-assisted myofascial mobilization and release techniques, such as Graston technique, for treating adhesions in the plantar fascia (Figure 3) and freeing the capsular ligaments of the hallux. Pin-and-stretch techniques applied to the plantar fascia and the muscles of the calf can also improve hallux motion.
Patients also should be taught to self-manage conditions like hallux limitus and hallux rigidus. Teaching them various ways to self-mobilize or stretch their hallux will aid in long-term relief and correction. The first self-treatment technique that we impart to patients is simply stretching the hallux into dorsiflexion. There are several ways to do this, but we do not have the space in this article to address them all.
[Editor's Note: Several other demonstration videos, including a video on stretching the hallux, accompany the app version of this article.]
Final Points / Considerations
While this article has discussed only one of the 33 joints found in the foot, we do not intend for the reader to treat this one joint in isolation. When we treat the hallux, we also evaluate every joint in the foot and the entire kinetic chain. We frequently will treat several other components of joint dysfunction in one patient.
Not every hypomobile joint should be adjusted. There are certain contraindications that should be respected: malignancy, bone disease, fractures, joint replacements or fusions, inflammatory joint disease (gout, RA) and joint ankylosis. Patients with these contraindications should not be adjusted.
Finally, the information in this article is not generalizable to other conditions of the hallux. For example, advanced hallux valgus, severe hallux rigidus, gouty arthritis, rheumatoid arthritis, and other inflammatory conditions should not be treated with high-velocity adjustments. Chiropractic adjustments may be provocative to these conditions, and prescribing an orthotic or obtaining protective footwear may be a good first step in conservative management.
Resources
- Cotterill J. Stiffness of the great toe in adolescents. Br Med J, 1887;1(1378):1158.
- Bergman T, Peterson D. Chiropractic Technique Principles and Procedures, 3rd Edition. Mosby; New York, 2010.
- Mennell JM. Joint Pain. Little Brown and Company, 1964.
- Root ML, Orien WP, Weed JH. Normal and Abnormal Function of the Foot - Clinical Biomechanics, Volume II. Clinical Biomechanics Corp. Los Angeles, 1977.
- Buell T, Green D, Risser J. Measurement of the first metatarsophalangeal joint range of motion. J Am Pod Med Assoc, 1988;78:439.
- Bojsen-Moller F, Lamoreux L. Significance of free dorsiflexion of the toes in walking. Acta Orthop Scand, 1979;50:471.
- Hetherington VJ, Johnson RE, Albritton JS. Necessary dorsiflexion of the first metatarsophalangeal joint during gait. J Foot Surg, 1990;29:218.
- Nawoczenski DA, Baumhauer JF, Umberger BR. Relationship between clinical measurements and motion of the first metatarsophangeal joint during gait. J Bone Joint Surg, 1999;81(3):370-6.
- Manral DB. Hallux rigidus: A case report of successful chiropractic management and review of the literature. J Chiropr Med, 2004 Winter;3(1): 6-11.