It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Piriformis Syndrome: Myth, Misdiagnosis or Just Rare?
OK, so I've hinted at my opinion already in the title. I am skeptical of piriformis syndrome (PS). I think it is a rare condition. When the concept was first birthed, it was based on the idea that there are causes of sciatica other than a herniated disc. At the time, within standard medical thinking this was an advance. I am using the term sciatica loosely, the way patients use it: any pain or abnormal sensation in the buttock, hamstring or posterior leg.
True discogenic sciatica is a much more clear-cut entity, with positive straight-leg raise, pain going below the knees, and dermatomal referral patterns. Many of your patients come in complaining of an achy buttock or strange sensations in the lower extremity, but do not have true discogenic sciatica. I am sure PS is diagnosed far more often than it should be.
Research suggests the piriformis is bisected by the sciatic nerve in only 17 percent of cases. Even more daunting, when surgery was done to free the sciatic nerve from purported piriformis entrapment, the piriformis was pierced by the nerve in only 16.2 percent of cases.1
Some recent research has been done on piriformis syndrome. Four features appear to be most common: buttock pain, aggravation of sciatica through sitting, external tenderness over the greater sciatic notch, and augmentation of the pain with maneuvers that increase piriformis muscle tension.2
The FAIR test is interesting. The test involves taking the lower limb into hip flexion, adduction and internal rotation, creating tension in the piriformis. Does this increase the symptoms? One attempt to verify the syndrome added testing the H reflex while doing the FAIR test. The working definition used these days does not appear to require the piriformis to be bisected by the sciatic nerve. It posits that other strains, or excessive tension in the piriformis or the other external rotators, can irritate or constrict the sciatic nerve.

My observation is that the term piriformis syndrome is used loosely and far too often by manual practitioners to diagnose the cause of buttock pain. This then leads the therapist to focus on stretching the piriformis and doing manual techniques to attempt to address the tight piriformis. This is usually done without a formal diagnosis and ignores what I believe are more common causes of buttock pain.
Here is what I think: Gluteal or buttock pain is common, and has many contributors and causes. Dysfunction of many structures can produce sclerotomal referral patterns into the buttock and legs. One of our strengths as manual practitioners is to recognize that most pain has multiple causes and contributors. One of our main jobs is to diagnose, tease out and address the multiple factors contributing to any painful condition. Pain is a liar, and many tissues create referred pain when they are irritated.
Check out this fascinating page describing Kellgren and Lewis's experiments, in which they self-injected hypertonic saline into muscles, tendons, ligaments and bones.3 If the piriformis is tight, I suspect it is an effect, rather than a cause. That doesn't mean it might not be useful to treat the piriformis area with various soft-tissue techniques. It does mean we may get more lasting results if we can figure out what else is contributing.
Six (of 10) Possible Causes of Buttock Pain
Let's examine the first six of 10 possible causes of buttock pain, and describe and attempt to differentiate each one. First, all of these are going to cause some variation on soft-tissue pain, with a bewildering variety of presentations and no easy, clear-cut answers. Carolyn McMakin's recent article in DC on "the challenging 20 percent" [April 15 issue, special section on managing pain] was an excellent overview of the underlying issues in chronic spinal pain.4
One of the things I love about being a manual practitioner is the opportunities to not only diagnose, but also to treat and observe changes. Using short therapeutic trials is a great way to get better as a practitioner, providing clearly targeted treatment. Here are the first six possible causes of a "pain in the butt."
1. Thoracolumbar Joint Dysfunction
This can cause irritation of the superior cluneal nerve, which provides sensory supply to the buttock. This phenomenon is so common, and yet so rarely consciously addressed. The superior cluneal nerve provides the sensory nerve supply to the flank and buttock. When they are irritated, the patient may complain of flank or buttock pain.
Don't miss this. The diagnosis is based on two factors: one is a palpable tender knot (Maigne's point), 7-8 cm lateral to the PSIS, on the upper glutes, just below the iliac crest; the second is joint restriction with significant restriction and tenderness (usually most obvious on the lateral margin of the involved spinous process), between T10 and L2. The solution is usually simple: mobilize the stuck joints. See Maigne's original work on this5 and read my article on this topic.6
2. Axial Discogenic Pain
Having just finished sitting for most of 27 hours while flying back from Australia, my left buttock aches. It will resolve in about three days, especially if I walk and decompress enough. Despite the fact that disc problems mostly cause lower back pain, rather than true nerve-root sciatica, they often secondarily refer into the buttock and thigh. Qualities of these patients include flexion intolerance (especially prolonged flexion), and improvement from decompression and extension. This diagnosis is often missed; many doctors think of the disc only in sciatica. This condition, whether we think of it as a torn disc or as pain from a degenerated disc, is common.
Unfortunately, it is difficult to have absolute clarity in diagnosis. As discograms are dangerous7 and MRIs don't reliably diagnose torn discs, it is realistically a preponderance-of-the-evidence diagnosis. (Note: These patients are flexion intolerant. The classic figure-four piriformis stretch, especially when done supine, can put them into lumbar flexion and irritate the disc, leading to lower back and buttock pain.8 Half the battle is stopping the patient from doing stupid stuff.)
3. Referral From the Key Ligaments of the Pelvis9
Pain is a liar. You might find the pain by overpressure or stretching the involved ligaments, but I tend to prefer palpation for tenderness and changes in tissue texture. Once in a while, palpation will create referred pain right to the area of pain; more often, you will just find tenderness.
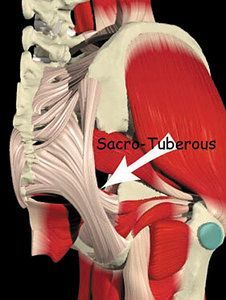
Often the key ligament is the sacrotuberous, either at its origin at the lower sacrum, or along its insertion. It is a frequent culprit, but is so rarely properly examined. The problem: The insertions of the sacrotuberous ligament are deep in the pelvis, where most practitioners are quite hesitant to touch. The sacrotuberous extends much further anterior than most texts show. When ligaments are tender, they are dysfunctional. The sacrotuberous often refers pain or abnormal sensation all the way to the ankle and foot.
Here is how to examine and treat the insertions of the sacrotuberous ligament. Tell the patient what you are going to do, and ask for explicit permission. Lay the patient on their involved side, bend the opposite leg up to 90-90, and rest the upper leg on a large pillow or bolster. Now, on the medial side of the lower thigh, slide your fingers anterior, starting at the ischial tuberosity and working your way anterior along the ischial ramus.
You are pressing in an inferior direction. You want your fingers to be directly in contact with the bone, where the ligament inserts. Where the ligament is tender, apply manual cross-frictional massage. I rarely use my metal tools here; it is too sensitive of an area. Do not be too vigorous or treat for over 2 minutes, especially the first time you do this on a patient. They can get very sore very easily.
4. The Internally Rotating Hip
This creates excessive length of the small muscles of the posterior pelvis,12 as emphasized in Shirley Sahrmann's model. The archetype would be the younger, female patient, with valgus knees, pronated feet and a hip that rotates inward too easily. Use a lunge test and watch for the valgus knee. The main thing to rethink is whether these muscles are tight and short, or long and weak.
When the hip rotates internally, the piriformis and its companion muscles will be over-lengthened and overstretched. An overstretched muscle can certainly feel tight to the touch. It can certainly have trigger points within it. It can feel good in the moment to stretch the area. But the common understanding of piriformis syndrome, that the patient needs to stretch the piriformis, is clearly wrong for the patient with an internally rotating hip.
Muscle testing, both functionally and directly, is useful here to assess for weakness of the glutes and piriformis. Instead of stretching, train the whole group, including the gluteus medius and gluteus maximus, for strength and motor control. Wake up the glutes; they are weak. Yes, go ahead and do your manual work, whether ART, Graston or manual release, but the key therapy is rehab exercise.
5. Evaluate the Sacroiliac
Emphasize the sacral side of the joint. When the sacrum is stuck, the piriformis will be unhappy. The sacral side of the joint is often missed here.13 (The exam findings are too complex for this article.) The piriformis does directly originate from the lower sacrum; if you are strictly correcting iliac misalignment, you will miss many significant dysfunctions.
In the muscle-energy system of osteopathy, a tight piriformis is one of the factors noted in an anterior sacral torsion. This is probably obvious to chiropractors, but the point is that the SI joint is a very important piece. Stuck joints will keep muscles from working correctly. The SI joint and its ligaments are important sources of referred pain into the anterior and posterior pelvis, and down the leg.
6. Let's Not Forget the Lower Lumbar Spine
The exam can include pain on extension or oblique extension, combined with motion palpation, as well as searching for tender points at the facet or over the spinous process. When L3, L4 or L5 are not moving well, the facet joints may refer to the buttock. Lumbar dysfunction will create or co-exist with muscular dysfunction around the core and pelvis.
In the second half of this article, I will explore four more sources of buttock pain, including the hip joint itself; the oversensitized sciatic nerve as a treatable entity; how core stability affects these patterns; and fascial restrictions affecting the lumbar and pelvic region.
The essence of my message is simple: When the patient has buttock pain, do not assume that either the nerve root or the piriformis muscle is the sole cause. Search for and treat the possible contributors.
References
- Smoll NR. Variations of the piriformis and sciatic nerve with clinical consequence: a review. Clin Anat, 2010 Jan;23(1):8-17.
- Hopayian K, Song F, Riera R, Sambandan S. The clinical features of the piriformis syndrome: a systematic review. Eur Spine J, 2010 Dec 19(12): 2095–2109.
- Altman LK. Who Goes First?: The Story of Self-Experimentation in Medicine. University of California Press, 1987.
- McMakin C. "The Challenging 20 Percent: Simplifying the Treatment of Chronic Pain." Dynamic Chiropractic, April 15, 2013.
- Maigne R. Low back pain of thoraco-lumbar origin. Arch Phys Med & Rehab, 1980;61:389-9.
- Heller M. "Thoracolumbar Junction or Superior Cluneal Nerve Entrapment Syndrome: : A Hidden Source of Low Back & Pelvic Pain." Dynamic Chiropractic, Nov. 4, 2011.
- Carragee EJ, Don AS, Hurwitz EL, Cuellar JM, Carrino JA, Herzog R. 2009 ISSLS prize winner: does discography cause accelerated progression of degeneration changes in the lumbar disc: a ten-year matched cohort study. Spine, 2009 Oct 1;34(21):2338-45.
- Heller M. "Stop Stretching - or at Least Stop Stretching the Lower Back Into Flexion and Rotation." Dynamic Chiropractic, Dec. 12, 2012.
- Heller M. "Sacroiliac Revisited: The Importance of Ligamentous Integrity." Dynamic Chiropractic, July 7, 2005.
- Hackett GS. Ligament and Tendon Relaxation (Skeletal Disability) Treated By Prolotherapy (Fibro-Osseous Proliferation). Charles C. Thomas Pub Ltd, 1958.
- Chart depicting ligament referral patterns: www.journalofprolotherapy.com/images/issue_02/prolo_for_pelvic_pain_figure_02.jpg
- Heller M. "The Internally Rotating Hip." Dynamic Chiropractic, July 29, 2009.
- Heller M. "The Sacral Side of the SI Joint: Correcting Anterior and Posterior Torsions." Dynamic Chiropractic, Dec. 16, 2010.



