It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Improving Posture: Create a 24/7 Bubble of Health & Function
No matter how well we've mastered our skills as chiropractors and no matter what techniques we use in our practice, our patients' patterned postural habits between office visits can dictate the level of success of our treatment plans.
One of my main motivations to become a chiropractor was my experience as an often-injured athlete. Innately, I was never satisfied with the symptom-oriented treatment the traditional medical model offered. I felt that given the right guidance, I could be doing things outside of the treatment and training room that would help my body heal faster and perhaps more effectively prevent future injury.
Score another win for innate intelligence! Over my many years in practice, and with the help and feedback from many incredible mentors, I've developed a "24/7 bubble" of healthy choices that I provide for my patients.
We become over time what we think, eat and do. As I observed patient after patient leave the office with reduced symptoms and increased function, I couldn't help but realize that many didn't even make it to their cars before reinforcement of pathological posture and faulty movement patterns began to undo the benefits of my care.
By the time I would see them a few days later, even if symptoms had subsided, it was apparent that their muscular imbalances, which more often than not were the actual cause of their condition, were recalcitrant to my attempts to correct them, even when the patient insisted they were doing their stretches and exercises.
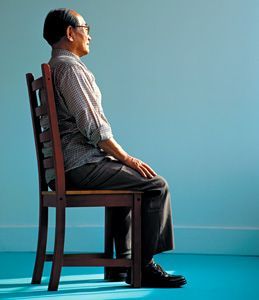
When I got the chance, I would try to spy on them as they drove away, and to my dismay, car seat after car seat would defeat their posterior chain and allow the classic deformation pattern of the sitting man: lumbar lordosis replaced by increased thoracic kyphosis. The hip flexors and hamstrings would shorten, and the abdominals would go on vacation. I would often use the classic line, "What are you doing to undo what I did, to undo what you're doing?" and remind them of the negative effects of sitting; "and when I say 'sitting,' that includes when you drive!"
I also knew that once they got out of the car, it wouldn't be too long before they found another place to sit and continued their daily process of rewiring the muscles in the front of the body to become overused, shortened and over time, affect movement and joint health, and cause their S-shaped spines to mold into the sad "C." A very real sign of the de-evolution of modern man.
Sitting Bull
Did you know that in the U.S., we sit 9.3 hours a day on average? Heck, we only sleep an average of 7.3 hours a night! Recent studies show the physiological effects of sitting are devastating to our overall health. When we sit for long periods, our mortality rate increases exponentially. And let's not forget that the no-so-attractive C-spine posture pattern also restricts respiration and compresses organs that were designed over millennia to function best while we are upright and in motion. Each time we sit, we reinforce "death by chair." Show me the people who live long, healthy lives, and I'll show you people who don't spend their days sitting.
"Posture Follows Movement Like a Shadow" – Sherrington, 1906.
But it's not just sitting. Our bodies are highly plastic and we mold to the posture and activities we do the most often. So, if our patients reach forward hundreds of times a day (at the computer, in the car or to pick up their kids), and never reach back in the opposite direction to exercise the muscles that hold them up, the countless repetitions in one direction create and feed imbalance and faulty posture. Imagine doing biceps curls all day and never activating the triceps or stretching the biceps. Where would your arm eventually end up? With your fist resting on your shoulder!
Poor posture when sitting also stimulates a sympathetic, fight-or-flight state that, among many other stresses, creates a measurable increase in deadly C-reactive proteins, significantly slows our metabolism, and negatively impacts cardiovascular health, immunity and digestion – and this is just the beginning of the list of poor posture's negative effects on overall health and wellness.
If your patients are looking for some perspective on observing posture and movement the way we (chiropractors) do in our "modern world," just have them watch how a 4-year-old moves and they will understand. Children move without restriction. Observe how a child squats and you will see a perfect hip hinge while they maintain their natural spinal alignment and curvature. They are using efficient, quality movement, the way we were designed to move. Just watch a young child get out of a chair and walk away, and then compare it to someone age 30 or older. If we sit an average of 9.3 hours a day, that means by the time we are 30, we have spent 84,862 hours sitting. It's a wonder we can still move at all.
In almost every case I've seen over the past 25-plus years, there are predictable muscular imbalances (think Vladimir Janda's upper-crossed syndrome) that have most likely been there for years, and have been reinforced by repetition of poor movement habits and postures that over time, limit function in mobility, stability and strength in the muscles that support and protect the health and function of the human spine.
That being said, what happens after your patient leaves the office is one of the greatest challenges to the success of your treatment outcomes. In my experience, along with the treatment we provide in the office, we must build our patients a 24/7 bubble of health, function and good choices for them to heal and flourish within, which also means the patient must be committed to taking an active role in improving and controlling their health, environment and decision-making process.
What You Can Do
- Tissue work. Lengthen and relax overused, understretched muscles and fascia for best treatment and training results. Always create tissue length before training for strength. Key muscles include the pec major, pec minor, subscapularis, upper lats, biceps, serratus group, upper traps and anterior scalenes.
- Mobilize/adjust the thoracic spine. Thoracic spine hypomobility exists in almost every patient; it increases instability in lumbar and cervical joints, and interferes with normal scapular and shoulder kinematics.
- Provide functional postural apparel and/or taping. Supports and cues proper posture and alignment by stimulating the sensorimotor system to retrain posture during activities of daily living. In short, it allows you to functionally reinforce the benefits of your treatment, posture and movement-training protocols.
What They Can Do
- Sit less. Use different styles of chairs that encourage movement, like a gym ball, yoga furniture, meditation pillows; and to get up and switch off every half hour. Get up and move more throughout the day. Adjusting position requires movement. They can also talk to their employer about ordering a stand-up desk. And encourage them to sit on the floor on a thick rug or carpet, with pillows for support, whenever possible.
- Improve workspace ergonomics. Use visuals; have someone take a picture of the patient in corrected posture. Place the picture of optimal posture in plain sight or tape to their computer monitor. Visual cues are also a powerful component you can use to create change of habit through constant reinforcement.
- Move better, move often. Age is not an excuse for poor movement and function; lack of movement is. Yoga, 5-rites, Pilates, tai chi and other exercise routines are fun and easy to follow. My strongest recommendation is to utilize foundation training. Check it out; it's a game changer because it focuses on improving posture and core strength by learning basic movements that activate and connect your posterior chain, from the Achilles to the occiput.
Maintaining optimal posture and balancing one's health is a journey, not a destination. Stress progress, not perfection! No matter the treatment method or modality you provide during an office visit, if you don't address functional balance by improving posture and quality of movement, and provide better choices for the environment the patient is living in outside your office, you'd better put on your running shoes. Why? Because then we become just one more symptom chaser in today's health care system and end up constantly repairing the effects of the posture and movement challenges patients face in the other 23 hours left in their day.


