It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Peripheral Sensory Nerves: A Treatable Source of Pain?
My last article was on thoracolumbar dysfunction as a source of superior cluneal nerve pain.1 In these cases, the patient will complain of lumbar and pelvic pain; but the source is the superior cluneal nerves at their origin at the thoracolumbar junction and along the nerves' course. Is this a common phenomenon, that sensory peripheral nerves get irritated and cause pain above and beyond the usual tunnel syndromes? I suspect that the answer is yes. I don't really know, but there are some tantalizing hints out there. If peripheral sensory nerves can and do cause pain, how do we diagnose and treat this?
One of the big questions is: When is peripheral nerve impingement the big issue and when is it not? On a bigger scale, that is the conundrum of chiropractic and manual therapy. We live in the gray zones. Musculoskeletal diagnosis is a challenging arena with relatively few definite answers. A true pathology, a single cause of chronic pain, is relatively rare. The usual scenario is a combination of contributions from dysfunctional joints, muscles, fascia and nerves. It is useful to recognize how little we know; what a "can of worms" pain is. I am always trying to use some kind of reality check, some kind of post-check, to know when I have made a significant change from whatever rehab, adjustment or soft-tissue work I have done.
Identifying and Addressing Peripheral Nerve Issues
We can find all kinds of lesions in the body, whether joint fixations or soft-tissue patterns. Figuring out which ones are significant is a more challenging issue. What got me excited about Maigne's model2 of superior cluneal nerve impingement is that he identified a point, 7 cm lateral to the midline just below the iliac crest, that appears to consistently identify a superior cluneal nerve impingement. Are there similar points throughout the body for other peripheral nerve issues? I suspect that these points are likely to be in or around tunnels and exit points of nerves. (If you know of them, let me know.)
Does Butler's type of nerve-tension testing give us a definitive diagnosis of nerve involvement? I don't think so, but it certainly adds another diagnostic test for the peripheral nerves. The testing is basically putting tension on the nerve with motion and positioning, and observing the patient's pain feedback. In my opinion, we do not have a definitive diagnostic test, a gold standard, for assessing peripheral nerve-mediated pain. The type of pain we are talking about might be better described as fascial impingements creating nerve irritation.
Butler3-4 and Shacklock5 have their own systems for addressing peripheral nerve tension. They use nerve gliding and occasionally a stronger stretch to the peripheral nerves, the goal being to free up the glide of the nerves within their sheath. Butler, in my limited reading of his work, seems to imply that the main therapy for most musculoskeletal pain is to glide the irritated nerves. Butler's main focus is on self-care; he shows the patient ways to glide their own nerves.
Barral has a whole system of manual therapy to the peripheral nerves.6 In his usual way, he is not interested in what others have figured out; he wants to create his own model. It is a useful system: basically applying a variant of myofascial release directly over the fascia surrounding the nerve.
In Barral's therapeutic sequence, he often starts with indirect, then finishes with direct. This means he starts by moving fascia over the nerve in the directions of ease, and after that begins to release, then takes it toward the barrier. This work is done very gently; you are not really tractioning the nerve. Start slow and don't force it. You really don't press deeply into the nerve tissue at all with this one.
Dry needling is another way to address peripheral nerve impingement. Inserting small-gauge solid needles (acupuncture needles) into areas that are restricted around the nerves seems to release the restrictions effectively. I have very limited experience with this technique, but it appears promising.
Another interesting view comes from John Lyftogt7-8 (pronounced Liftoff). The first reference is an overview of Lyftogt's view of chronic pain, as central sensitization versus peripheral nerve issues. The second reference is a discussion of back pain and treatment by neuro-prolotherapy. Lyftogt is an MD in the prolotherapy tradition who has come up with another way to treat chronic pain. He feels that most chronic pain is not from central sensitization, but from peripheral nerve issues. His treatment is to inject a 5-percent glucose solution around the nerve. (I wonder whether dry needling would produce the same result.)
The purpose is to quiet the nerves causing the pain. He calls his work neuro-prolotherapy, but it is quite a different model than traditional prolotherapy. He is not attempting to create first-stage healing of ligaments and tendons; he is attempting to quiet the nerves.
Clinical Observations
What happens to the tissues that surround impinged nerves? Here are my clinical observations. The fascia, the connective tissue, surrounding the irritated nerve get gooey and stuck, and quit moving normally. How can we restore normal movement? Active release technique (ART) talks about releasing the fascia around the areas where nerves get impinged. FAKTR adds dynamic movement models to the instrument-assisted soft-tissue approach, which could be helpful for these conditions. The osteopathic approaches, including Barral's and Barnes' myofascial release, use slow, gentle fascial methods.
Are there simple, quick ways to release these peripheral nerve impingements? For certain impingements, such as Maigne's syndrome (lumbar or pelvic pain secondary to thoracolumbar restriction), the answer appears to be spinal manipulation. This implies that the tender points on the buttocks in Maigne's syndrome are either a double crush or strictly a referred pain phenomenon creating distal trigger points. If it is a true double crush, then it would be useful to treat both the spinal source and the distal area with some sort of manual therapy. As DCs, we are familiar with double-crush syndromes. We always look at the spinal origins in peripheral pain syndromes.
I suppose that I am particularly fascinated by this topic at least partially due to my own experience. My chronic back pain was markedly improved by a methylene blue injection into my L4-5 disc, which attempts to kill the pain-causing nerves that have invaded the disc. (Unfortunately, this therapy seems to be much less effective in the U.S. than it was in the original Chinese studies. The docs I know who tried it out have dropped it.)
What I do know is that if you can quiet pain, the patient gets better in remarkable ways. We all know this from watching our own patients' behavior. The obvious improvements include improved mood and affect. The other significant factor is how core muscles can finally start functioning when the pain diminishes.
Plotting a Course of Care
So, what is the take-home information from this discussion? First, go back to your anatomy texts and look at the nerves and the surrounding tissues. Think about which peripheral sensory nerves supply which areas. Second, check out the joints from which these peripheral nerves begin. If they are restricted, release the joints and the surrounding fascia. Third, "trace" the nerves. Are they abnormally sensitive to the touch? Is the sensitivity at particular locations? Exit points and tunnels are typical places for fascial restriction to affect the nerve. If so, figure out a way to release these, whether with gentle myofascial or deeper fascial work, or your laser or e-stim device. When you change tenderness, you may change pain patterns.
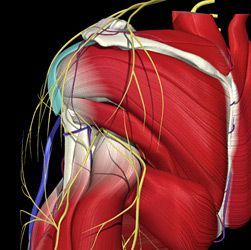
Here is an example. Let's take the axillary nerve. Its sensory branches supply the skin over the shoulder. It is supplied by the spine at C5 and C6, from the posterior trunk of the brachial plexus. It exits to supply the skin through the quadrilateral space, where the nerve could get impinged. This space is found below the teres minor, above the teres major, lateral to the triceps, medial to the humerus.
You could check C4-5, C5-6 and C6-7 for fixation, and correct that. You could do gentle or vigorous fascial release around the quadrilateral space. You could very gently traction with two contacts: one on the lateral side of the lower cervical spine and the other over the quadrilateral space. If you are attempting to do it like Barral would, use 20 percent of your normal force and start very slowly. Begin by gently engaging and then listen, follow.
Pain is a liar. Keep searching. Keep your mind open to new ideas. Keep asking yourself: What can be the cause of pain in this particular puzzling case?
References
- Heller M. "Thoracolumbar Junction or Superior Cluneal Nerve Entrapment Syndrome: A Hidden Source of Low Back and Pelvic Pain." Dynamic Chiropractic, Nov. 4, 2011.
- Robert Maigne. The French Society of Orthopaedic and Osteopathic Manual Medicine. See his four articles on the thoracolumbar junction. www.sofmmoo.com/english_section/accueil_english_section.htm
- Butler DS. Mobilisation of the Nervous System. Churchill-Livingston, 1991.
- Nee RJ, Butler DS. Management of peripheral neuropathic pain: integrating neurobiology, neurodynamics and clinical evidence. Physical Therapy in Sport, 2006;7:36-49.
- Shacklock M. Clinical Neurodynamics: A New System of Neuromusculoskeletal Treatment. Elsevier, 2005.
- Barral J-P, Crobier A. Manual Therapy for the Peripheral Nerves. Churchill-Livingston, 2007.
- Lyftogt J. Pain conundrums: which hypothesis? Central nervous system sensitization vs. peripheral nervous system autonomy. Australasian Musculoskeletal Medicine, November 2008;13(2):72-4.
- Lyftogt J. Prolotherapy for recalcitrant lumbago. Australasian Musculoskeletal Medicine, May 2008;13(1):18-20.


