It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
What Is Low-Force Chiropractic? Palpation, Adjusting and Soft-Tissue Applications
I want to talk about the initial touch we use when we palpate, when we adjust, and when we do soft-tissue therapy. The bottom line is that most of us tend to be too harsh. It's all about the first contact you make with the skin and muscles underneath. When you first touch the body, what is the quality of your touch? If you start gently and then increase your pressure as you need to, you will elicit a whole different response. You can push too hard just as easily with an instrument-assisted device as you can with your hands.
We are the experts in high-velocity, low-amplitude thrust, the classic chiropractic adjustment. I think this quick thrust predisposes the rest of our touch toward quick, deep and hard.
I have always focused on what is the safest, lowest-risk way to both assess and treat. As someone who touts low force, I tend to hear the horror stories from patients who were injured by a chiropractic adjustment. I know what we do is relatively safe, but how can we make it as safe as possible without compromising effectiveness?
I am fortunate to have studied with osteopaths, and especially with the French osteopaths. My teachers were masters of a soft and gentle touch. I have come to realize how much information the body can reveal to me with a soft touch.
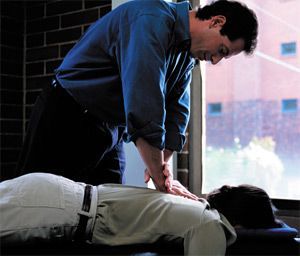
When you palpate, when you line up the body for an adjustment, when you start to probe deeply or superficially into the soft tissue, there really is a better way. Start gently, start gradually and sink into the tissue, instead of gouging into the tissue. Hey, I have to admit that when I get in a hurry, I don't always walk the low-force walk.
I have alluded to the initial touch for palpation. This article is inspired by a Rolfer I work with. Rolfing is known for being deep and intense. This particular Rolf practitioner has a wonderful skill of knowing how to start gently, how to engage the tissues, how to get the patient to relax. All of this makes her deep work much more tolerable.
Applications for a Low-Force Approach
Who needs this more gentle initial approach? One obvious group would be those who have suffered recent trauma and are especially sensitive. For this type of patient, the nervous system is already in overdrive; they are already supersensitive. Don't set them off by immediately increasing their pain. For anyone with any posttraumatic stress, a harsh touch, sudden movements, the sound of the joint popping; all of these may set them off.
How many of our patients, at least in their injured areas, are storing some posttraumatic stress? Older folks need everything done a little slower and a little gentler. They just don't adapt or change as easily. What about your new patient? They do not know what to expect; they come in with a bit of fear, conscious or unconscious. Start gently, let them relax, and you are likely to have a better response.
As long as I am generalizing, let's add anyone in pain to our list. Pain ramps up the nervous system, and you don't want to create any additional painful experiences for the person in pain. And what about any patient who has experienced childhood trauma or abuse? This group tends to misinterpret touch quite easily. With these folks, you not only need to be gentle; you also need to be extremely clear with your words, your focus and your intent, to make them feel safe.
Let's talk about that 800-pound gorilla in the corner. That would be strokes caused by upper cervical manipulation. Even though we know that the literature says this is extremely rare, and almost random; even though we know it may be more likely to happen when the person turns their head to look down the street than during / after an adjustment. I am talking about perception here, and the special responsibility we have as doctors.
Do you have a way to adjust the upper cervical spine other than high-velocity, low-amplitude? In our office, the default is the low-force methodologies, especially in the neck. I ask the patient what works better for them. If they know that HVLA is what works best for them, that is what I will do. If they prefer low force, I have a whole set of tools for that. If they don't have a clear preference, I will use the low-force methods and reassess to see if I have normalized the joint motion. If I have not, I will consider recommending an HVLA thrust.
Low Force Applied to Palpation
I love motion palpation; the essence of what we are doing is to assess for lack of motion and to restore motion. Allow me to suggest a small but profound way to change what you are feeling for: As you sink into the tissue, feel for the first barrier. (I discussed this back in 2002; read "A Different Way to approach the Barrier: Initial Response Testing" in the July 30, 2001 issue.) What is the quality of the motion as you begin to move the joint? You are assessing the "beginning feel" rather than just the "end feel." The lack of motion, the stiffness of abnormal tissues, can be felt as soon as you start to move the tissue.
This is a radical idea. I invite you to try it out. Just slowly move the joint or press toward the barrier. How soon can you feel the restriction? By the time you reach end feel on a symptomatic restricted joint, you will have created pain for the patient. At beginning feel, the patient usually will not experience pain. If you are trying to prove to them that this is "their spot," creating pain temporarily may be useful. If you are trying not to ramp up their pain response, don't create pain.
Low Force Applied to the Adjustment
Whatever adjusting technique you are using, you can apply these low-force concepts. If you are doing an HVLA thrust, just start with a slower, more gradual setup. Continue with allowing the patient to relax in the setup. You may find that you do better by not taking the joint all the way to the end of motion, and then thrusting. You may find that backing off just a bit allows for an easier adjustment. You will have to play with this to get the idea.
The other aspect of low-force HVLA is in finding the minimal force necessary to move the joint. I was privileged to have Joseph Howe, DC, a renowned chiropractic radiologist, as one of my teachers at National. Although Dr. Howe did not teach adjusting, somehow he ended up one day showing us how he adjusted the cervical spine. He was so gentle; he used just enough force. This was an amazing teaching moment for me. It was so different, such an epiphany, that I clearly remember it 33 years later.
Using low-force techniques is a whole different game. In the chiropractic profession, we tend to think of this as instrument adjusting. In the rest of the manual therapy world, including osteopathy and physical therapy, low-force work is hands-on. I primarily use techniques that were pioneered by early osteopaths. Your patients will love these. My patients routinely say something to the effect of, "I didn't know you could adjust me so easily, so painlessly."
These techniques include muscle energy (post-isometric relaxation applied to joints), and counterstrain (indirect, fold and hold). On the neck, I use a lot of what I call "engage, listen, follow." This is basically direct three-dimensional myofascial release applied to the stuck joint. (Read "Adjusting Techniques, Part Two, Including ELF and Recoil,"; in the Sept. 1, 2001 issue.)
I noticed that when I first learned muscle energy, I wanted to lock out the joint at the end range. The better muscle energy practitioners use the slack, allowing a little more play, which allows the joint to move more easily. When you use muscle energy, you are retraining the small stabilizer muscles around the joint, as well as moving the joint.
One criticism of low-force adjusting techniques is that the actual adjustment does not create as much afferentation; it does not fire off the joint receptors as strongly. This is inherently true. The patient may not get the "buzz" of an HVLA adjustment. The question I would ask is this: What is the long-term change in the afferentation of the joint receptors? Deafferentation means the brain is not getting enough signals from the joint receptors because the joint is stuck and not moving, thus not firing the joint receptors. An HVLA adjustment does give a large and sudden spike to these joint receptors.
But is that our primary job? I think our job is to restore motion and to train the patient to continue to move properly, thus restoring afferentation. The jury is out on what kind of adjusting does this best. Very few studies have compared techniques. As a practitioner, my job is to find out what works for the patient on my table; the patients in my practice. Individualize your care to your patient, with the goal of restoring normal motion. This will involve your adjustments, your soft-tissue methods and rehab; how you teach the patient to continue to move.
Low Force for Soft-Tissue Work
Soft-tissue methods could be divided into two quite distinct types. One is inherently low force; variations on myofascial release. This is usually done with quite low pressures; although the term myofascial release means different things to different practitioners.
The other category of soft-tissue release starts, in our profession, with Raymond Nimmo, DC, who pioneered receptor-tonus technique, and includes Janet Travell's trigger-point therapy. We could go on to include Graston Technique and fascial manipulation. All of these use a heavier pressure. Earlier in my career, I focused on the lighter soft-tissue methods; more recently, I've come to appreciate the deeper forms and the opportunity to start up first-stage healing they allow.
You can start any soft-tissue method with a gentler entry. When you are doing Graston, use lighter strokes first. When you are pressing deeply, as in trigger-point therapy or fascial manipulation, begin with a lighter touch and gradually increase your pressure. Once you are deep, ask the patient to rate the pain you are creating. Ask if the pressure is tolerable or intolerable. Find a level they can tolerate – maybe a 7 out of 10 depending on the patient. If the patient is writhing on your table, you may be using too much pressure. Remind the patient to keep breathing and to relax into your touch. Yes, you can do deep-pressure soft tissue with a lighter touch.
I know I am standing on my soapbox in this article. I hope this overview is useful. I have just scratched the surface on this topic. Low-force manual methods have been the underlying theme of my whole series of columns over the past nine years. The take-home in this article is to ask yourself: How much pressure is needed? How is the pressure being applied: gradually or suddenly? Your patients will appreciate it when you are a bit more gentle.


