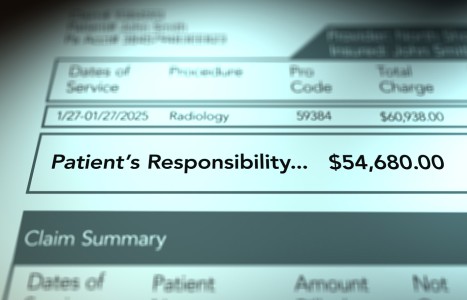
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Medicare and the Chiropractic Practice, Part 5
Near the end of our last article (Jan. 1 issue), we indicated that contractors must evaluate suspected claims errors through the use of "probe" reviews. Under probe reviews, contractors may initially examine 20-40 claims per provider for provider-specific problems. Contractors may also conduct widespread probe reviews (involving approximately 100 or more claims from multiple providers) when a larger problem, such as a spike in billing for a specific procedure, is identified. In either type of review, providers are notified that a probe review is being conducted and are asked to provide medical documentation for the claim(s) in question. Providers are then notified of the results of the probe review.
When probe reviews verify that an error exists, the contractor classifies the severity of the problem as minor, moderate or significant. Contractors may classify the severity of the error by determining the provider-specific error rate (number of claims paid in error), dollar amounts improperly paid, and/or past billing history. All levels of error will require that providers receive education on proper billing procedures and the collection of money from claims paid in error. Contractors will then respond to the billing problem(s) as appropriate for the level of severity,and determine what steps need to be taken to correct the problem(s).
Often, initial medical review (MR) is conducted by simply examining the claim itself, usually in an automated method. If more information is needed (a small percentage of cases), the contractor will request access to medical records to confirm that the services rendered are reflected on the claim, coded correctly, and covered by Medicare.
Validating initial findings from MR evaluations may require additional reviews resulting in corrective action. To assist in MR evaluations, CMS designed MR Progressive Correction Action (PCA), which ensures that MR activity is targeted at identified problem areas and that imposed corrective actions are appropriate to the severity of the infraction of Medicare rules and regulations.
Postpayment review is generally performed by using statistically valid sampling. Sampling allows an underpayment or overpayment (if one exists) to be estimated without requesting all records on all claims from providers. This reduces the administrative burden for Medicare and costs for both Medicare and providers. Both prepayment and postpayment reviews may require providers to submit medical records. When medical records are requested, the provider must submit them within the specified time frame or the claim(s) will be denied as having no documentation. Provider feedback and education regarding MR findings are essential elements of all corrective actions. Feedback and education further ensure proper billing practices. The purpose of the MR process is to make sure claims are paid correctly. DCs need to take certain measures to help meet this goal:
Providers should also keep in mind the following points:
The provider has the right, following MR, to be educated on how to bill correctly and to have questions answered in a timely manner. The provider also has the right to appeal determinations, as long as the appeals are filed in accordance with regulations governing that process. After claims have been reviewed, the provider will be notified of the result of the review (full denial, partial denial, or favorable/no denial). In the first two cases, full or partial denials, the contractor may decide to recoup the reimbursement from the provider (if the provider accepts assignment) or from the patient (if the provider does not accept assignment), with instructions to seek reimbursement from their provider. The provider must then reimburse the patient. It is at the time of receipt of these denials that the provider may choose to appeal. The next article will summarize the appeals process. The reader is reminded that while we recommend and encourage all DCs to appeal improperly denied claims, we do not recommend or encourage the frivolous appeal of claims. Appealing is not only a service to your patient, who has a right to have their payable covered services reimbursed, but also a service to your profession. March 2010
Trending
Personal Injury / Legal
Jeff Randolph, Esq.;
Michael Coates
With estimates showing over 30 million Americans affected by peripheral neuropathy – and a significant portion underdiagnosed – it’s increasingly likely that chiropractors are already treating these patients. What’s missing is structured recognition, comprehensive management and targeted tools to slow progression, improve function and support systemic health.
Christopher Proulx, DC, PhD(ABD), CSCS
Billing / Fees / Insurance
Each year, ICD-10-CM is updated on Oct. 1. For 2026, there are 74,179 total codes, with 487 additions, 28 deletions and 38 revisions. Code changes are based on date of service, not the claim submission date. Services performed on/after Oct. 1 must use the new codes. While no changes affect the common spinal or extraspinal codes most frequently used by DCs, several updates may still affect your claims – particularly for comorbidities, referred pain, or trauma cases. | Digital Exclusive
Samuel A. Collins
|