Some doctors thrive in a personality-based clinic and have a loyal following no matter what services or equipment they offer, but for most chiropractic offices who are trying to grow and expand, new equipment purchases help us stay relevant and continue to service our client base in the best, most up-to-date manner possible. So, regarding equipment purchasing: should you lease, get a bank loan, or pay cash?
Rehabilitation of the Rodeo Athlete
The rodeo contestant represents a unique athlete, distinguished by distinctive social demographics,1 physical characteristics2,3 and types of injures encountered.4-8 Kotarba1 describes the rodeo cowboy as a rugged individual whose sports' subculture supports a system of health care that is inexpensive, nonmedical in its philosophy, personalistic in the structure of its practitioner-patient relationship, and incidental in its delivery. Mindful of these observations, it is interesting to note how the rodeo athlete has quickly accepted the type of care chiropractors can offer. The primary group delivering chiropractic care at the rodeo event is based in Tacoma, Wash., currently under the direction of Ed Corley, DC.

Visionary members of the ACA Sports Council conceptualized this type of chiropractic care in the early 1990s. In 1992, members of the Tacoma-based group began working rodeo events and it quickly became apparent that these services were in demand. The over-abundance of events and injured contestants proved useful in the training of novel sports doctors and in the maturation of confidence that has helped nurture the chiropractic profession's insertion into other sporting events. The team-oriented, complementary, and collaborative medical affiliation of professionals has demonstrated its clinical effectiveness not only in rodeo, but also has been identified by Meeker and Haldeman9, and Smith, et al.,10 as fundamental for the profession to thrive and grow in today's complex health care matrix.
Risk of Injuries
Butterwick, et al.,5 recently performed a prospective longitudinal study of professional rodeo contestant injuries in Canada. The study ran from 1995 through 1999 and involved 63 rodeo events; 451 injuries were reported during 30,564 competitor-exposures. The most injuries occurred in the rough-stock events (bull riding, bareback riding and saddle bronc [Figure 1]). Meyers, et al.,8 reporting on collegiate rodeo athletes in the National Intercollegiate Rodeo Association (NIRA) Southern Region, found that rodeo athletes face an 89 percent probability for injury per season. Further, there is a 6:1 potential for injury among rough-stock events.
Rehabilitation and Sport-Specific Care of the Rodeo Contestant
Recent demographic information and overall physical activity levels recently were reported on 72 male Professional Rodeo Cowboys' Association members by Sinclair and collegues.2 Sixty-two percent of the subjects participated in regular exercise for a minimum of two days per week. This low level of sport-specific training may play a part in an inverse relationship with injury rates. This suggests chiropractic efforts are needed beyond the manipulative level of care.
The injured rodeo contestant is classified into one of three rehabilitative groups at the beginning of care. Triano, et al.,11 describe the rehabilitative groups as protective, active and resistive.
Protective: These patients are in acute pain. Treatment is focused on decreasing symptoms and introducing preliminary exercise programs focusing on flexibility and early aerobic activity.
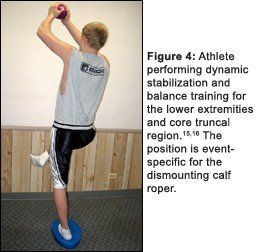
Resistive: Pain is minimal and the athlete's functional level is high. Much of the rehabilitative effort is being performed by the patient on their own time and likely in their own gym. Minimal contact with the provider is needed at this stage of convalescence. Advanced levels of instruction are given on dynamic stabilization and injury prevention for their specific event.
Case Report
A 37-year-old calf roper presents with low back pain. Duration is one month. Onset was insidious and pain intensity is rated 4/10 with an "ache" character. The athlete is neurologically intact, and has full lumbar range of motion with pain re-created on extension at L4-S1. Normal muscle strength to the lower extremities is found and normal posture is observed on inspection. He denies bowel and bladder symptoms.
Two areas of concern are identified in the history. First, the low back pain and associated stiffness are slowly worsening. Second, his event times have slowed, making it nonprofitable to be on the road as a professional athlete.
Diagnosis: Facet Syndrome
Therapy is initiated by first categorizing the athlete into one of the above-listed rehabilitative stages. In this case, the patient was placed in the active stage. Manipulation with physiotherapy was started to begin addressing the pain complaints. Haas, et al.,12 documented how the combination of manipulation and physiotherapy modalities will accelerate recovery. Time is a major factor in dealing with a disabled worker or, as in this case, the professional athlete with a limited season of competition. Aerobic activity of 20 minutes per day was initiated, along with strengthening and flexibility exercises.
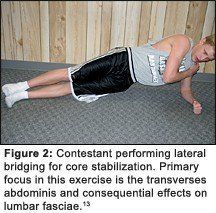
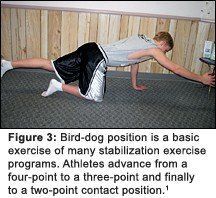
The patient was in the active stage of rehabilitation and we aggressively started core stabilization (Figures 2 and 3, illustrating lateral bridging and bird-dog position, respectively) and proprioceptive training (Figure 4, athlete balancing on labile surface with right foot elevated) on this first day as well.
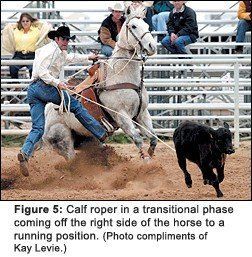
The objective of a chiropractic rehabilitative sports program is to focus beyond the athlete's pain and address event performance in treatment goals. As in the above case, the calf roper did experience low back pain abatement and improvement in event times. The outcome was consistent with pre-treatment goals. The athlete was dismissed to an independent exercise program, where he continued his various forms of exercise to promote core stabilization, flexibility, aerobic involvement and strength.
References
- Kotarba JA. Conceptualizing sports medicine as occupational health care: illustrations from professional rodeo and wrestling. Qual Health Res 2001;11(6):766-79.
- Sinclair AJ, Ransone JW. Physical activity and its relationship to rodeo injury and success. J Strength Cond Res 2004;18(4):873-7.
- Meyers MC, Wilkinson JG, Elledge JR, Tolson H, Sterling JC, Coast JR. Exercise performance of collegiate rodeo athletes. Am J Sports Med 1992;20(4):410-5.
- Meyers MC, Sterling JC, Souryal TO. Radiographic findings of the upper extremity in collegiate rodeo athletes. Med Sci Sports Exerc 2003;35(4):543-7.
- Butterwick DJ, Hagel B, Nelson DS, LeFave MR, Meeuwisse WH. Epidemiologic analysis of injury in five years of Canadian professional rodeo. Am J Sports Med 2002;30(2):193-8.
- Butterwick DJ, Meeuwisse WH. Effect of experience on rodeo injury. Clin J Sport Med 2002;12(1):30-5.
- Ketai LH, Temes RT, Deis JL, Allen NL, Wernly JA. Rodeo related large animal injury: is protective head-gear warranted? Injury 2000;31(10):757-9.
- Meyers MC, Elledge JR, Sterling JC, Tolson H. Injuries in intercollegiate rodeo athletes. Am J Sports Med 1990;18(1):87-91.
- Meeker WC, Haldeman S. Chiropractic: a profession at the crossroads of mainstream and alternative medicine. Ann Intern Med 2002;136(3):216-27.
- Smith M, Greene BR, Meeker W. The CAM movement and the integration of quality health care: the case of chiropractic. J Ambul Care Manage 2002;25(2):1-16.
- Triano JJ, McGregor M, Skogsbergh DR. Use of chiropractic manipulation in lumbar rehabilitation. J Rehabil Res Dev 1997;34(4):394-404.
- Haas M, Groupp E, Kraemer DF. Dose-response for chiropractic care of chronic low back pain. Spine J 2004;4(5):574-83.
- Barker PJ, Guggenheimer KT, Grkovic I, et al. Effects of tensioning the lumbar fasciae on segmental stiffness during flexion and extension: Young Investigator Award winner. Spine 2006;31(4):397-405.
- Akuthota V, Nadler SF. Core strengthening. Arch Phys Med Rehabil 2004;85(3 Suppl 1):S86-92.
- Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med 2006;34(3):445-455.
- Arokoski JP, Valta T, Kankaanpaa M, Airaksinen O. Activation of lumbar paraspinal and abdominal muscles during therapeutic exercises in chronic low back pain patients. Arch Phys Med Rehabil 2004;85(5):823-32.



