Some doctors thrive in a personality-based clinic and have a loyal following no matter what services or equipment they offer, but for most chiropractic offices who are trying to grow and expand, new equipment purchases help us stay relevant and continue to service our client base in the best, most up-to-date manner possible. So, regarding equipment purchasing: should you lease, get a bank loan, or pay cash?
Revisiting the Scaphoid Fracture
When a patient presents with a history of a fall on an outstretched hand and there is pain at the wrist, the bony integrity of the carpals and distal radius should be foremost on the clinician's mind. Although there commonly will be pain and possibly swelling with no bony injury at all, it is prudent to conduct a thorough evaluation of all bones at the wrist, in particular the scaphoid. Due to the frequency of scaphoid fractures, the fact that they can be occult, and are plagued with complications, makes this injury a significant concern in wrist trauma patients.
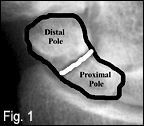
The scaphoid is the most frequently fractured bone in the wrist1-3 and accounts for 50 percent of all carpal fractures.2 The anatomical location at the lateral border of the wrist articulating with the distal radius makes this bone a point of stress during a fall on an outstretched hand. During this mechanism, the wrist is in varying degrees of hyperextension while there is downward force from the radius. Scaphoid fractures typically occur between the ages of 15 and 40 years and are unusual among children.1-3 The fractures are classified by their location: proximal pole, waist, distal body and tuberosity. Some authors simplify the classification by combining the distal body and tuberosity into the distal pole (see figure 1). Localizing in which portion of the scaphoid the fracture occurs will assist in determining the likelihood of ischemic necrosis, non-union and the rate of healing.1

There is a dual blood supply to the bone, with a vessel at the distal pole and another in the region of the waist. When a fracture occurs at the waist, it is more likely to impact the blood supply to the proximal portion of the bone. Because the blood supply enters at the waist, fractures here and more proximally put the fracture fragment at an increased risk for ischemic necrosis (see figures 2 and 3). Approximately 70 percent of all scaphoid fractures occur at the waist; 20 percent occur at the proximal pole and the remaining 10 percent occur at the distal pole.1-3
In general, fractures at the distal pole have a better prognosis than those at the waist or proximal pole. Up to 15 percent of scaphoid fractures will develop ischemic necrosis.1-3 In addition, anywhere from 15 percent to 30 percent of fractures will have non-union.1-3 The proximal pole has the highest incidence of non-union. For those fractures that become non-union, there is an increased incidence of ischemic necrosis - approaching 30 percent to 40 percent.1 The time required for healing varies according to location. Fractures at the tuberosity (distal pole) usually heal in four to six weeks, whereas fractures at the waist or proximal pole may require up to eight weeks or longer.1

One of the main concerns is the fact that a significant percentage of scaphoid fractures are occult, meaning they are not visible on radiographs at the time of injury. Up to 30 percent of scaphoid fractures may be occult.2 The fact that they are not radiographically detected sometimes leads to poor management which increases the risk for ischemic necrosis or non-union. When the radiographs appear normal and there is pain at the anatomical snuffbox, the wrist should be immobilized and repeat X-rays performed in 7 to 10 days.2 A phase of fracture healing during which there is resorption of the fracture site will occur, making it visible on radiographs at this time. While most fractures should be visible within 7 to 10 days, another study shows that fractures, if present, will likely be visible 20 days after the injury.2 If there is confirmation of a fracture, an appropriate orthopedic referral can be made for assessment and permanent casting. In addition, if no fracture is identified at this time, it is likely one does not exist and less conservative treatment can be initiated.
Advanced imaging can play an important role in detecting a scaphoid fracture if there is strong clinical suspicion with negative plain-film radiographs. Some studies suggest the loss of productivity from erroneously immobilizing a patient is more costly than performing an MRI to make a definitive diagnosis.2 Both bone scan and MRI will be abnormal in patients with occult scaphoid fracture.2 MRI is the most sensitive imaging modality for the early detection (24-48 hours) of ischemic necrosis, even more so than a bone scan.3 MRI is more accurate in defining the location within the scaphoid than a bone scan, but both have near-equal sensitivity in detection after 72 hours.2
For patients in whom a scaphoid fracture has been detected, it is important to completely assess the wrist and elbow, as there are, on occasion, associated injuries to a scaphoid fracture, such as fractures of the radial styloid process, triquetrum or capitate; Colles' fracture; ligamentous disruption; or fracture to the radial head.1
Clearly, the scaphoid fracture is one of the most complicated wrist injuries that can be encountered in the chiropractor's office. Even once detection occurs, there is still risk of ischemic necrosis or non-union. After four to eight weeks of healing and freedom from any complications, full rehabilitation can be initiated, along with chiropractic adjustments to the area. At times, surgery will be necessary to combat the non-union or address the bone and joint changes associated with ischemic necrosis. Mismanagement of the occult fracture needs to be minimized, particularly in such litigious times.
References
- Resnick D, G Niwayama. Diagnosis of Bone and Joint Disorders, 3rd ed. Philadelphia: W.B. Saunders, 1995.
- Yochum T, L Rowe. Essentials of Skeletal Radiology, 3rd edition, Baltimore: Williams & Wilkins, 2005.
- Marchiori, D. Clinical Imaging With Skeletal, Chest and Abdomen. St. Louis: Mosby, 1999.