It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Anterior Cruciate Ligament Injury: Pre- and Postoperative Rehabilitation (Part 1 of 2)
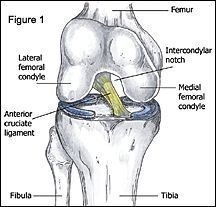
The anterior cruciate ligament (ACL) is a tough fibrous structure that attaches the tibia (lower leg bone) to the femur (thigh bone) (Figure 1). This ligament helps stabilize the knee by preventing excessive forward movement of the tibia on the femur. ACL injuries commonly occur in athletes participating in sports such as football, basketball, soccer and volleyball, in which movements such as cutting, pivoting, single-leg landing and rapid decelerations are routinely performed. Tearing of the ACL is most commonly caused by landing awkwardly, or cutting on a fully extended or slightly flexed leg with the foot turned outward (Figure 2).

Skiers usually injure the ACL when they catch the inside edge of a ski on ice, causing them to lose control and fall backward as they hyperflex the knee. The injured athlete may report hearing a "pop" and say it felt as if the knee was being stretched apart. Examination of the knee may reveal extensive swelling around the knee joint, loss of full extension of the knee and an inability of the athlete to bear weight on the injured leg. Manual testing may reveal excessive forward movement of the tibia on the femur.
Once the athlete is diagnosed with an ACL injury, the first step is to decide whether to undergo surgery to reconstruct the torn ligament, or to rehabilitate the knee without surgery. ACL reconstructive surgery is only recommended for athletes who continue to suffer from repetitive bouts of the knee giving away, or for those athletes who want to return to a highly competitive sport level. Athletes deciding not to have reconstructive surgery may be able to return to an active lifestyle after completing a rehabilitation program; however, they must learn to modify their activities to accommodate for the compromised stability of the knee due to the lost check-rein function of the ACL.
Preoperative rehabilitation is important for those athletes who choose to undergo surgical reconstruction. The main goals of the preoperative rehabilitation protocol are to reduce swelling around the knee joint, and to restore full range of motion and functional strength to the injured limb. The preoperative rehabilitation phase prepares the patient physically and mentally for both the surgery and the postoperative rehabilitation program.
Postoperative rehabilitation begins immediately after surgery. The most important goals in the first two weeks are to reduce swelling and restore full range of motion of the knee in extension and flexion. Once range of motion is restored and swelling is minimized, the progression of the postoperative program depends on the patient's determination, level of swelling and pain, and the clinician's knowledge of the normal biological progression of healing of the reconstructed ligament. Some athletes progress rapidly in the post-operative phase of rehabilitation and may begin sport-specific training at a low intensity level in two to three months. However, full functional rehabilitation of the reconstructed ACL may not occur until six to 12 months postoperatively. The therapist must be careful about the progression of the rehabilitation exercises and the timetable for returning the athlete to his or her particular sport. An accelerated rehabilitation program under a controlled environment allows the athlete to return to sport sooner, without increasing the risk of complications.
Origin and Insertion Points of the Anterior Cruciate Ligament
The bottom of the femur consists of the medial and lateral femoral condyles, circular bony protuberances that are separated by an intercondylar notch. The top of the tibia consists of the medial and lateral tibial plateaus: flat ,slightly concave surfaces that articulate with the respective femoral condyles. The anterior cruciate ligament originates from the posterior outer aspect of the intercondylar notch and proceeds anteriorly, where it inserts onto the outside edge of the medial tibial plateau. See Figure 1.
Graft Tissue Healing Post-Surgery
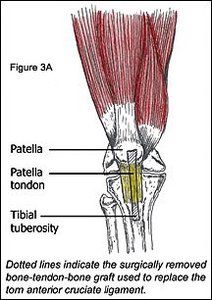
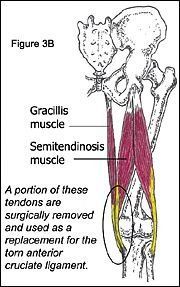
In athletes, a torn anterior cruciate ligament is typically removed and replaced with tissue of their own that is similar in length and strength. The two most common self-tissue grafts are the bone-tendon-bone (specifically, tibial tuberosity bone - patella tendon - patella bone graft) (Figure 3A), and the hamstring tendon graft (specifically, the tendons of the inside hamstring muscle [semitendinosis], and adjacent groin muscle [gracillis]) (Figure 3B). The selected graft tissue would be surgically placed in the anatomical location of the previous ACL, and then secured by interference screws.
Both types of grafts have advantages and disadvantages. The surgeon selects the appropriate type of surgery based on the patient's sport and the movements most frequently used.
A study by Rodeo, et al., evaluated tendon-to-bone healing in a dog model and found that a firm attachment of tendon to bone occurred at 12 weeks post-surgery. At two weeks post-surgery, there was still no continuity between the graft tendon and the insertion point in the bone. At four weeks, there was minimal continuity between tendon and bone. At eight weeks, there was considerably improved continuity between tendon and bone. After 12 weeks, the tendon graft was safely secured to the surrounding bone, at which point failure of the graft-insertion point was minimal.
Based on the results of the above study, from zero to four weeks post-surgery, therapy should focus on decreasing inflammation and restoring full range of motion of the knee. Swimming, stationary cycling, isometric contraction exercises, and other low-force muscle integrating techniques can be implemented in the earlier stages of rehabilitation. If the patient experiences pain, swelling or decreased range of motion of the knee, the inflammation should be reduced, range of motion restored, and the intensity of the rehabilitation phase should be slowed down. During the 12-week healing period, a skilled therapist should carefully monitor exercise selection to reduce the risk of complications.
Rehabilitation of the Knee: Decrease Swelling and Restore Range of Motion
Rehabilitation after ACL reconstruction surgery should initially focus on decreasing inflammation and restoring normal range of motion. Every patient heals differently; the progression of the rehabilitation program should be customized to the athlete and progressed to his or her tolerance.
Initially, decreasing inflammation around the knee joint using ice, compression, and elevation is feasible with a couple of icepacks, an ace bandage, and pillows to prop the leg up. Ice therapy should be maintained 20 minutes on and one hour off, multiple times per day. Ankle pumps (flexion and extension of the foot) with the leg elevated can be conducted five minutes per hour to further reduce swelling. A cryotherapy cuff, if available, is a more advanced method of decreasing inflammation. The device can be wrapped around the knee and filled with ice water. A cooler of ice water is attached by tubing to the cuff and can be used to replace the old water in the cuff with ice-cold water every hour. Anti-inflammatory medication is also useful in reducing swelling around the knee joint.
The next couple of steps of the postoperative phase should be conducted to the patient's tolerance.
The patient should use crutches following the first two days post-surgery, with minimal weight-bearing. Additional weight may be applied to the injured leg, with crutches, as tolerated. By the end of the first week, the patient may ambulate without the support of crutches if a normal walking gait cycle with full weight-bearing can be sustained with no noticeable instability. The patient should be able to ambulate without crutches six to seven days postoperatively.
Restoring full range of motion of the injured knee, particularly in extension, should be a priority in the first two weeks post-surgery. After the first week of postoperative rehabilitation, the patient should be able to fully extend and flex the leg to 110 degrees. At this point, full extension is the most important goal; flexion of the knee improves steadily as swelling around the knee joint decreases. If full extension of the knee is not restored within two weeks post-surgery, scar tissue may develop in the joint, preventing the restoration of full knee extension.
The continuous passive motion machine (CPM), an electrical motor-driven device, may be used in the hospital immediately following recovery from surgery. This machine has shown promise in helping to restore normal motion and flexibility of the injured leg. The CPM supports the leg while moving it from full extension to a progressively set degree of flexion. There is a 10-second pause at the end of each movement, during which time the patient will isometrically contract the quadriceps (front thigh muscles).
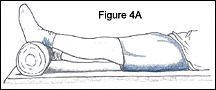
After the patient is released from the hospital, a specific series of exercises (provided by a trained therapist) should be done as often as possible to restore full range of motion of the knee in extension. Passive extensions (Figure 4A) and weighted extensions and prone leg hangs (Figure 4B) are useful exercises for restoring extension of the knee. During passive extensions, the patient can lie on the back with the heel propped up on pillows. Once the leg is relaxed in extension, the patient can periodically contract the quadriceps musculature to push the knee further into extension. The patient then holds the quadriceps contraction for five seconds, and then returns to relaxed extension. This exercise should be done for 15 minutes and repeated every waking hour. If extension is not achieved this way, the patient may progress to weighted extension exercises by placing a 5-10 pound weight just above the knee and following a similar procedure as passive extensions. The patient should be instructed to perform this exercise for 10 minutes, taking the weight off for one minute and repeating multiple times during the day. Prone leg hangs (Figure 4B) can also aid in restoring extension of the knee. Have the patient lie on the stomach with the knee just past the edge of the table or bench with the knee in full extension; use a weight if struggling with full extension. The patient should perform this exercise for 10 minutes, gently flexing and extending the knee and repeating multiple times per day.

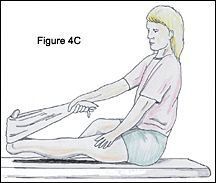
Towel stretch extension exercises (Figure 4C) can be incorporated if the above exercises are not restoring extension appropriately. The patient sits on a bench, places a towel around the foot of the injured leg, and applies tension to the towel to dorsiflex the foot, pulling the toes backward. The patient then raises the heel off of the ground to bring the knee into extension, while placing the other hand on the thigh to stabilize the leg.
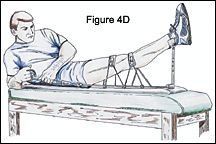
A device such as that shown in Figure 4D can also be used to forcefully restore extension of the leg. This is to be used if extension of the leg is not restored before two weeks post-surgery. The patient lies down on the back with the ankle raised and secured into a heel rest; a pad would be placed above and below the knee joint. These pads are secured by ropes passing through a ratchet system that would be tightened to force the knee into full extension.
A normal gait cycle depends on a person's ability to lock the knee in full extension while weight bearing. The following resistive tubing exercise can aid in accomplishing this goal. Resistive tubing can be secured above the standing patient's kneecap and anchored to a bench behind the patient; the resistive force of the tubing will promote full extension while standing.
Heel slides, supine leg hangs, and prone flexion exercises with a flexible band (Figures 5A, 5B, and 5C) can be used to restore flexion of the injured knee. Heel slides are conducted with the patient lying on the back, sliding the heel toward the buttocks until tension is felt; the position is then held for one to two minutes. The heel then slides down into full extension. This exercise should be repeated 10 times, once every waking hour. See Figure 5A.

Supine leg hangs are conducted with the patient lying on the back, grasping the hands behind the thigh and lifting the thigh toward the chest with the leg flexed. The patient then allows the leg to drop down into flexion, holding this position for two minutes. The knee is then returned to a relaxed extended position. This should be repeated multiple times throughout the day. See Figure 5B.
Prone (on the stomach) flexion exercises can be conducted with the flexible band. Starting out on the back, the patient creates a toe loop with the band around the injured knee's foot, and then turns onto the stomach. The band is then swung over the head, slowly increasing the band's tension, hand over hand, while the ankle is aligned to the buttocks. The stretch should be held for three to four minutes, repeated several times throughout the day. See Figure 5C.
Joshua C. Dubin, DC, CSCS, CCSP
Quincy, Massachusetts



