It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
The Condyle Subluxation
The condyle subluxation is a misalignment presentation that is rarely discussed in the pediatric population, but may often have serious ramifications for infants and young children.
One of the earlier pioneers who taught the evaluation and adjustment of pediatric condyle subluxation was Clarence Gonstead. Herbst later described Dr. Gonstead's teachings in a pediatric chapter in 1968.1
This article is written to introduce the reader to the evaluation of and set-ups for the condyle misalignment. It is not a substitute for the in-depth discussion and pictorial presentation found in the textbook Pediatric Chiropractic.2
The AS (anterior and superior) condyle may occur with in utero constraint (transverse, brow or facial presentation) or forehead/brow extension injury. Some physical manifestations that may be related to the AS condyle are low APGAR score at birth, weak cry, poor thriving abilities, cerebral palsy, and autism.
The PS (posterior and superior) condyle, which is more common, occurs when a child's head is in flexion during a fall or other injury. Possible symptoms related to this presentation include headaches, vertigo and other symptoms similar to an atlas subluxation.
The condyle subluxation may be evaluated with inspection, static and motion palpation, and radiographs.
Inspection of the condyle misalignment should be performed with the patient in an upright, weight-bearing position. The normal observation is a horizontal gaze. The infant or child should be viewed from the lateral position. The position of the skull in an inferior tilt may suggest the PS condyle, whereas a superior head tilt may indicate an AS condyle.
Static palpation provides limited information for identifying the AS condyle; however, the PS condyle will reveal edema or muscle bulging on the side of laterality (LS or RS). Contact is made with the fifth or second digit on the posterior-inferior aspect of the occiput.
Motion palpation provides a valuable tool for assessing flexion and extension range of motion. The doctor should contact the condyle with his or her fingertips and laterally flex the patient's head to one side slightly, in order to isolate the articulation. Once the joint is isolated, introduce the rocking motion of flexion and extension. The PS condyle will manifest fixation during extension; the AS condyle will manifest during flexion.
The condyle subluxation may be confirmed with radiographic studies. The relationship of the occiput and atlas is analyzed with the lateral neutral film.3 The AS or PS condyle will reveal deviation of the foramen magnum line and the atlas plane line. This may also be confirmed with stress radiographs. The flexion view is performed to confirm the AS condyle, and the extension view for the PS condyle. The APOM film is used to determine side of laterality (LS or RS) and axial rotation.
It is recommended that the PS condyle adjustment be performed with the patient in the seated position. The infant can be placed between the thighs of the doctor; the older child can sit in a chair. Chest stabilization may be achieved by the parent's hand contacting the child's chest. The PSLS or PSRS (lateral flexion dysfunction) will be corrected by contacting the supramastoid groove on the side of laterality. The doctor should use the distal end of his or her thumb to contact the infant, and the thenar eminence to contact the older child. The doctor's stabilization hand supports the cervical musculature on the opposite side.
Figure 1 reveals an infant PSRS. The pattern of thrust for the PSLS listing is posterior to anterior, superior to inferior, right to left, through the C0-C1 joint plane line, with an infe-riorward arcing motion toward the end of the thrust. Figure 2 shows a child set-up for the PSRS. The pattern of thrust is the same.


The patient position for the AS condyle is the seated position. The supine position may be used for a newborn or handicapped child who may not have the developed cervical musculature to be placed in the seated position. A condyle block is used in all AS condyle adjustments. The condyle block is placed behind the cervical spine (C1-C7) to prevent introduction of flexion during the thrust phase.
Figure 3 shows the infant placed in the lap of the doctor. The doctor interlocks his or her fingers and contacts the glabella. The doctor's elbow stays close to the body. The pattern of thrust for the AS condyle is anterior to posterior, superior to inferior, with an inferiorward arcing movement across the lateral mass of C1.

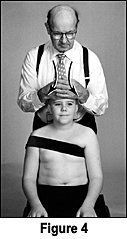
Figure 4 shows the older child in the seated position. The flat palm of the doctor's hand will contact the center of the glabella and supraorbital margin. The opposite hand will overlap the contact hand for stabilization. Pre-tension at the joint is obtained with slight head flexion.
For the supine AS condyle adjustment, the infant is placed supine with the crown of the head placed closed to the edge of the table. Depending on the doctor's height, he or she will kneel or squat at the end of the table. Figure 5 depicts a thenar eminence contact on the glabella.

Due to the frequency of falls and tumbles during children's first few years of life, chiropractors should expand their evaluation of pediatric patients to include the condyle region. Early detection and correction may prevent a host of childhood clinical symptoms.
Author's note: All photographs in this article courtesy of Lippincott Williams & Wilkins.
References
- Herbst RW. Gonstead Chiropractic Science and Art, chapter 19. Sci-Chi Publications, Mt. Horeb, WI, 1968:261-268.
- Anrig C, Plaugher G. Pediatric Chiropractic, chapter 9. Lippincott Williams & Wilkins, 1998.
- Ibid, chapter 8.
Claudia Anrig, DC
Clovis, California