It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Visual Recovery Following Chiropractic Care -- Part II
This article on visual changes following manipulation was very well received. I say this by judging the number of responses this article has created. Thank you.
J. Vollers, D.C., Whittier, California, was one of the first to reply, and in his letter he relates a common experience. "I personally have been involved in a particular case where following an auto accident a 45-year-old woman's vision changed (worsened) to 20/400 from 20/20. The patient sought care at the prestigious Jules Stein Vision Center (UCLA) where nothing was found to explain her vision problem. Four weeks later I saw her and began manipulation and traction therapy. Within five days her vision returned to 20/20. I would like to add that I saw a patient who eight months before had lost her voice after an auto accident. The EENT specialist had given up on her case. After one week of manipulation and cervical traction her voice returned to normal."
How Is this Relationship between Manipulation and Impaired Vision Explained?
This is a most interesting question, especially from my perspective as the professor for the course "Eyes, Ears, Nose, and Throat." In order to expedite the search for answers to this question, I tapped into the services of CHIROLARS. Sure enough CHIROLARS found what we needed -- articles discussing improved vision following manipulation.
There are at least four theories discovered in my search. Let's take a look at them:
The Barre-Lieou Pain Syndrome
The syndrome of Barre-Lieou is often referred to as an explanation for many of these visual incidents. According to the original authors, the syndrome may affect any part of the head and neck, and the symptoms are classified as follows:1
- pharyngeal and laryngeal syndrome
- facial syndrome
- aural and vestibular syndrome
- pseudocardiac syndrome
- ocular syndrome
The latter involves the changes believed to occur with trauma to the cervical soft tissues. This theory rests upon the principle of facilitation wherein it is suggested that there is facilitation of the sympathetic innervation to the blood vessels of the optic nerve creating just enough ischemia to impair, but not stop, transmission of visual stimuli.
Decreased Acuity Due to Disturbance in Sympathetic Tone
Visual acuity is highly dependent upon the precise function of all the components of the focusing mechanism. In other words, decreased precision in function translates into decreased acuity. Here again, the sympathetic system is brought into play. It is known that changes in sympathetic tone affect the tonus of the fine muscles controlling the iris and the lens. This, in turn, may disrupt visual acuity. You may have heard the expression, "I was so scared, I couldn't see straight." Fear, in this case, strongly stimulated the sympathetic system.
Orthodromic and Antidromic Activation of Sensory Fibers in the Trigeminal Pathway
A third theory can be constructed from the recent discovery of dual sensory-efferent function of certain primary neurons.2 The demonstration of the existence of sensory-efferent function of certain nerves has added new dimensions to the possible role played by these neurons in the pathogenesis of head pain complaints. Through this third theory, orthodromic and antidromic activation of sensory fibers of CN V may, in fact, give rise to many symptoms associated with the visual mechanism.
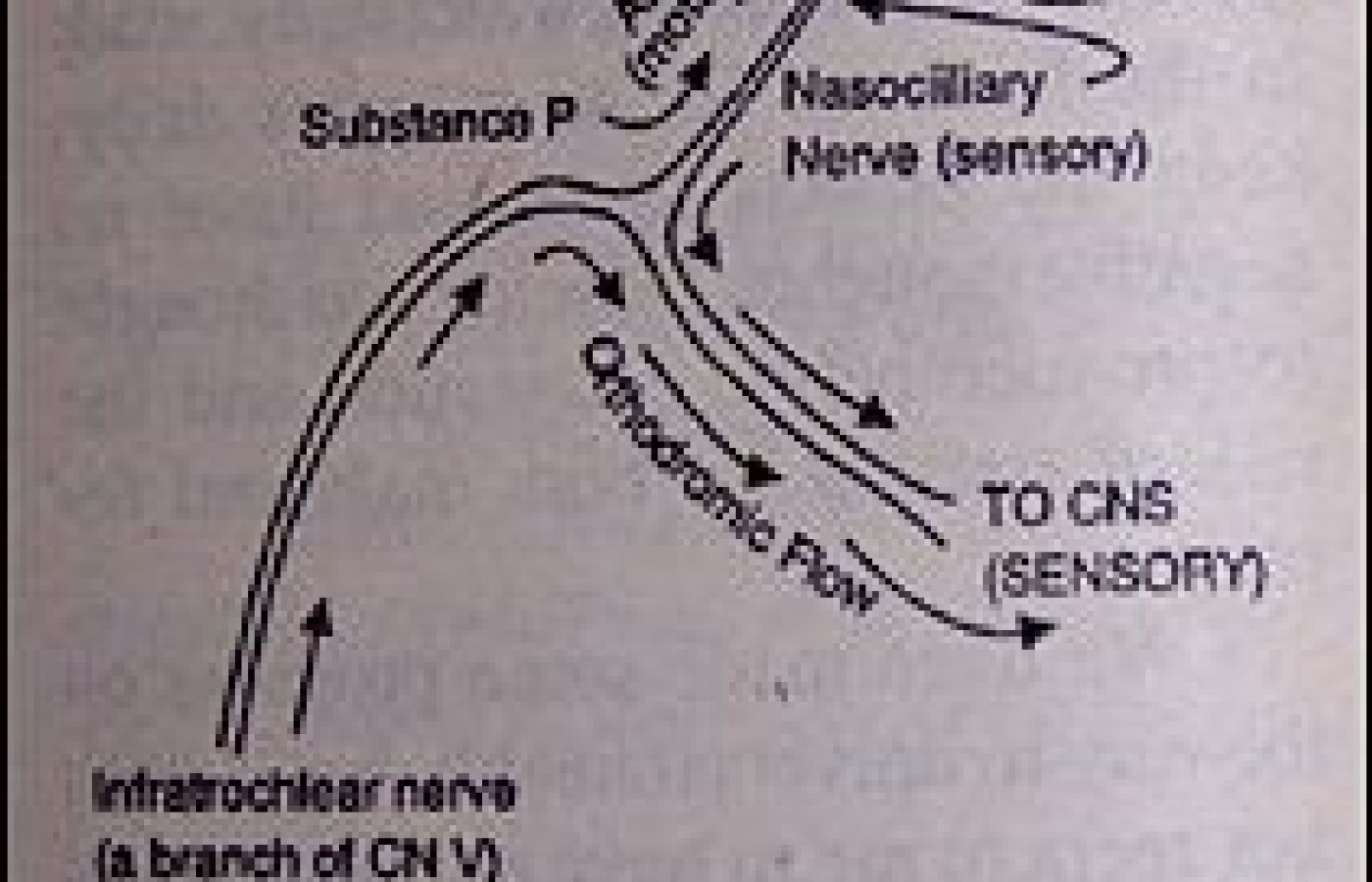
In this context, we will look at the iris, a target organ involved in certain visual disorders, which is known to be stimulated by antidromic activation of sensory fibers of CN V. The neurotransmitters, in this case, are substance-P and neurokinin.
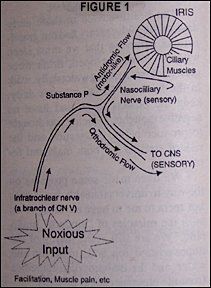
Evidence clearly indicates that the ocular response to mechanical or electrical stimulation of the trigeminal nerve is analogous to that produced by local trauma. It can be assumed that there is diffusion of peptides (substance-P and neurokinins) that are released antidromically from sensory nerve endings, and these peptides activate muscle receptors (in this case the ciliary muscles of the iris) which produces miosis.
This particular pathway would be activated through an axon reflex which involves: 1) noxious input, e.g., facilitation from motor dysfunction; 2) afferent fibers of the infratrochlear nerve; 3) collateral nerves from the nasociliary nerve supplying the muscle of the iris.
Visual Change Is a Serendipitous Event
A fourth interpretation used to explain visual recovery is simply that the recovery is serendipitous. In other words, it is possible that there is not a cause-and-effect relationship between chiropractic intervention and visual recovery.
References
- Gairal L: Toulouse, The Barre-Lieou syndrome. New York State J Med., 53:13, July 1951.
- Fanciullacci M, et al: Unilateral impairment of pupillary response to trigeminal nerve stimulation in cluster headache. Pain, 36:185-191, 1986.
With each article I encourage you to write the questions you may have, commentaries on patient care subsequent to attending the TM seminars, or thoughts to share with your colleagues, to me:
Darryl Curl, D.D.S., D.C.
2330 Golden West lane
Norco, California 91760
Please enclose your return self-addressed, stamped envelope.
Editor's Note:
Dr. Curl will be teaching MPI's Temporomandibular ("TM") seminar on May 9-10, 1992, in Cincinnati, Ohio. You may register for the seminar by dialing 1-800-327-2289.