It’s a new year and many chiropractors are evaluating what will enhance their respective practices, particularly as it relates to their bottom line. One of the most common questions I get is: “Do I need to be credentialed to bill insurance, and what are the best plans to join?” It’s a loaded question – but one every DC ponders. Whether you're already in-network or pondering whether to join, here's what you need to know.
Simple Low Back Pain: Rest or Active Exercise?
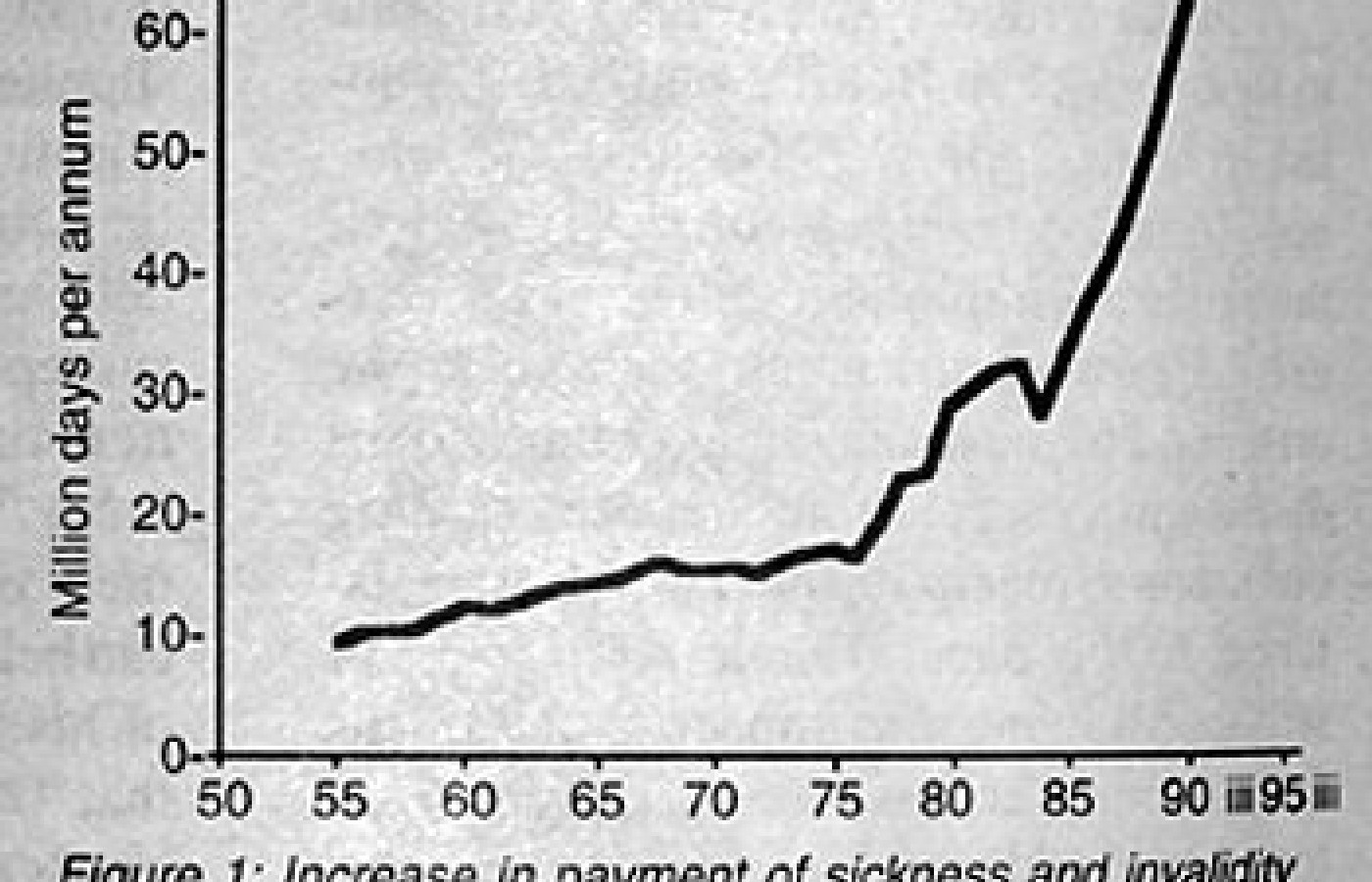
Back pain is not new; it has been reported throughout recorded history.1 Nor is there evidence of any change in the nature or severity of back pain. What is new is the scale of chronic disability due to simple backache. The latest Department of Social Security statistics for 1990-1 (Fig. 1) show that back pain now accounts for 67 million days of sickness and invalidity benefit each year in the United Kingdom and is the second most common cause of physical disability after cardiovascular disease. Moreover, it is increasing faster than any other form of chronic disability and has increased by 13% in the last year. Nor is there any evidence of change in the biological basis of back pain. What has changed in our understanding and management of this common bodily symptom. With the introduction of the disease model of illness in the 19th century, three key ideas laid the foundation for what is now traditional treatment for low back pain: that it comes from the spine; that it is commonly caused by injury; and that the basic strategy of management should be rest.
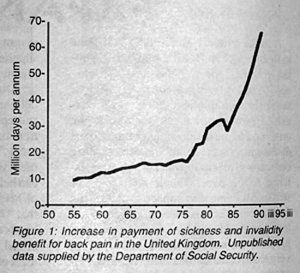
Figure 1: Increase in payment of sickness and invalidity benefit for back pain in the United Kingdom. Unpublished data supplied by the Department of Social Security.
Therapeutic rest for back pain was first introduced by the newly emerging specialty of orthopaedics.2 Previously, the sick bed had always been regarded as a consequence of serious disease rather than a treatment.3 Since that time, rest has become the traditional treatment for low back pain. Indeed, the most recent edition of one of the standard undergraduate textbooks of orthopaedics4 actually still advocates: 'the principle is to provide rest for the lumbar spine ... [either] by a plaster jacket or bed rest ... rest for the spine must be continued for 6 to 12 weeks according to progress.' In a postgraduate education questionnaire,5 67% of general practitioners in the United Kingdom selected bed rest as the 'correct' treatment for a 38 year- old man with a two week history of simple low back pain.
The rationale of rest for low back pain is not nearly as obvious as might be imagined. It appears to be a mixture of ideas based on a disease model of the spine and ignoring the physical and biopsychosocial effects on the patient. The main concepts are: the painful spine is irritable; movement and physical activity will increase pain and hence must be harmful; diagnoses of 'disc' problems -- biomechanical studies show that disc pressure is lowest when supine, so that somehow the disc will 'go back' by lying down; and the orthopaedic principle of therapeutic rest. None of these concepts has pathological validity for simple low back pain.
Conversely, the ill effects of rest are part of standard medical and nursing teaching. Prolonged bed rest is the most effective method known of producing a severe disuse syndrome.6 We no longer use prolonged rest to treat any other condition and go to considerable lengths to avoid it. Nor does the scientific evidence support bed rest for low back pain or even sciatica. There are now five controlled trials of bed rest for low back pain.7-11 The only trial to suggest that bed rest was better than staying ambulant8 had serious methodological defects. The two most carefully designed and executed trials showed that two days of bed rest for low back pain were better than seven days of bed rest, whereas no bed rest at all was better than four days of bed rest. Deyo et al.10 showed that patients with acute low back pain given medical recommendation of two days of bed rest returned to work significantly faster than those recommended seven days of bed rest. Gilbert et al.9 showed that those who received no bed rest reported significantly less restriction of daily activities and returned to normal levels of activity significantly faster than those instructed to stay in bed for at least four days. No trial showed any adverse effects of earlier mobilisation. There is no evidence comparing bed rest in hospital with bed rest at home. So in these days of increasing demand for the cost effective use of resources it is difficult to justify the admission of 40,000-50,000 patients to hospital each year in the United Kingdom for bed rest for low back pain and sciatica.
There is increasing evidence that low back pain and disability are better understood and managed according to a biopsychosocial model12 (Fig. 2). Viewed from this perspective, there are strong theoretical arguments against bed rest and for an active exercise approach to low back pain and sciatica. Physically, this will prevent the disuse syndrome and promote the natural history of recovery. Perhaps even more importantly, it will minimise the harmful cognitive, affective, behavoural, and social effects of assignment to disability status. These theoretical arguments are supported by solid scientific evidence. There are now 18 published controlled trials of an active exercise approach for low back pain13-31 (reviewed by Waddell12). Fourteen of these trials show statistically and clinically significant benefits in pain, disability, physical impairment, cardiovascular fitness, psychological distress, or work loss.
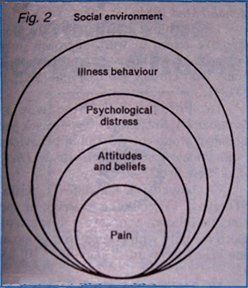
Figure 2: Biopsychosocial model of low back pain and disability.
Fundamental questions remain. Koes et al.32 found little evidence favouring any specific type of physiotherapy exercise. The benefit appears to lie in an active exercise approach with the emphasis on increasing physical activity and return to work. Most of the trials considered chronic low back pain, though a well designed and executed trial by Lindstrom et al.31 showed that the same approach can be applied successfully at the six week stage. Moreover, the control groups in the bed rest trials7,9-11 confirm the advantages of early mobilisation in patients with acute low back pain. There is still no doubt about the most effective methods of achieving this strategy. The key treatment elements in the trial by Lindstrom et al.31 were measurements of functional capacity, an incremented exercise programme, an operant conditioning behavioural approach, and rehabilitation directed towards return to work including a workplace visit. This reduced the average duration of work loss from 15:1 to 10 weeks and reduced the number of patients progressing to chronic invalidity from 4/52 to 1/51. Some trials, however, have shown that improvements are maintained for at least six months to two years,15-17,19,21,30,31 whereas others have found that initial improvements regress after a few months.22,24,25,28,29 There is no evidence that earlier return to work predisposes to recurrence or 're-injury.' On the contrary, Lindstrom et al.31 showed that the active group still had significantly less work loss due to low back pain in the second year of follow up. Doubt also remains about the mechanism of these effects. Some of the improvements seen in performance occur too rapidly to be physiological. It is not clear to what extent successful rehabilitation is primarily physiological or behavioural. Further trials are required in the early stages of acute low back pain and in sciatica. Most importantly it remains to be proved whether comparable results can be achieved in community health care delivery.
There is now sufficient evidence to demand a fundamental reappraisal of our basic strategy of management for low back pain. The Agency for Health Care Policy and Research in the USA and the United Kingdom Clinical Standards Advisory Group are currently considering management guidelines for low back pain. The choice is clear: rest or active exercise? The scientific evidence is also clear. Many patients with low back pain may need to modify their activities temporarily in the acute stage. A few patients may require one to three days of bed rest for acute low back pain or up to two weeks for nerve root pain. Rest, however, is better regarded as an unfortunate and undesirable consequence of acute pain, not as a treatment. Bed rest should be avoided whenever possible and always ended as rapidly as possible. The prescription of rest and restricted activity for chronic pain is absolutely contraindicated. There is now good evidence for an active exercise approach for chronic low back pain. There is strong theoretical argument for, some scientific evidence for, and no evidence against a similar approach to acute low back pain. The same principles probably apply, though over a slightly longer time scale, to nerve root pain.
We are now facing an epidemic of lower back disability in all western societies. Traditional medical treatment has not halted this epidemic and may even have contributed to it. We need a new strategy of management directed equally to pain and disability, which places equal emphasis on the symptomatic relief of pain and restoration of function. We need a community health care delivery system which achieves this in practice, within the first three months before chronic pain and disability become established. This requires changes in how patients, doctors, and society deal with low back pain. The prime responsibility lies with doctors who not only provide medical advice and sick certification for low back pain, but also provide society with the concept and understanding of low back pain on which our whole management system is based. If this analysis is correct, the first step to halting this epidemic requires a radical change in medical thinking and practice. Such change in the behaviour of doctors is always difficult to achieve,33 but if we continue as we are doing it appears likely that low back disability will continue to increase. From the present statistics, that is the inescapable challenge of low back pain in the last decade of the 20th century.
- Allan DB, Waddel G. An historical perspective on low back pain and disability. Acta Orthop Scand Suppl 1989; 234: 1-23.
- Thomas HO. Contributions to surgery and medicine. London: Lewis, 1874.
- Sydenham T. The whole works of that excellent physician Dr. Thomas Sydenham. 10th ed. London: Feales, 1734 (Translated by John Pechey).
- Adams JC, Hamblen DL. Outline of orthopaedics. 11th ed. Edinburgh: Churchill Livingstone, 1990: 184-90.
- PGEA questionnaire. Medical Monitor 1992 Sep. 11.
- Bortz WM. The disuse syndrome. West J Med 1984; 141: 691-4.
- Coomes EN. A comparison between epidural anaesthesia and bed rest in sciatica. BMJ 1961; 1: 20-4.
- Wiesel SW, Cuckler JM, Deluca F, Jones F, Zeide MS, Rothman RH. Acute low back pain. An objective analysis of conservative therapy. Spine 1980; 5:324-30.
- Gilbert JR, Taylor DW, Hildebrand A. Clinical trial of common treatments for low back pain in family practice. BMJ 1985; 291: 791-4.
- Deyo RA, Diehl AK, Rosenthal M. How many days of bedrest for acute low back pain? N Engl J Med 1986; 315: 1064-70.
- Szpalski M, Hayez JP. How many days of bedrest for acute low back pain? Objective assessment of trunk function. European Spine Journal 1992; 1: 29-31.
- Waddell G. Biopsychosocial analysis of low back pain. Clin Rheumatol 1992; 6: 523-57.
- White AWM. Low back pain in men receiving workmens' compensation. Can Med Assoc J 1966; 95: 50-6.
- Dehlin O, Berg S, Andersson GBJ, Grimby G. Effect of physical training and ergonomic counseling on the psychological perception of work on the subjective assessment of low back insufficiency. Scand J Rehabil Med 1981; 13: 1-9.
- Catchlove R, Cohen K. Effects of a directive return to work approach in the treatment of workmens' compensation patients with chronic pain. Pain 1982; 14: 181-91.
- Fordyce WE, Brockway JA, Bergman JA, Spengler D. Acute back pain: a control group comparison of behavioural vs. traditional management methods. J Behav Med 1986; 9: 127-40.
- Mayer TG, Gatchel RJ, Kishino ND, et al. Objective assessment of spine function following industrial injury: a prospective study with comparison group and one-year follow-up. Spine 1985; 10: 482-93.
- McCain GA, Bell DA, Mai FM, Halliday PD. A controlled study of the effects of a supervised cardiovascular fitness training program on the manifestations of primary fibromyalgia. Arthritis Rheum 1988; 31: 1135-41.
- Hazard RG, Fenwick JW, Kalish SM, et al. Functional restoration with behavioural support. A one year prospective study of patients with chronic low back pain. Spine 1989; 14: 157-61.
- Reilly K, Lovejoy B, Williams R, Roth H. Differences between a supervised and independent strength and conditioning program with chronic low back syndromes. J Occup Med 1989; 31: 547-50.
- Linton SJ, Bradley LA, Jensen I, Spangfort E, Sundell L. The secondary prevention of low back pain: a controlled study with follow-up. Pain 1989; 36: 197-207.
- Harkapaa K, Jarkikoski A, Melin G, Hurri H. A controlled study on the outcome of inpatient and outpatient treatment of low back pain. Scand J Rehabil Med 1989; 21: 81-95; 1990; 22: 181-94.
- Turner JA, Clancy S, McQuade KJ, Cardenas DD. Effectiveness of behavioral therapy for chronic low back pain: a component analysis. J Consult Clin Psychol 1990; 58: 573-9.
- Deyo RA, Walsh NE, Martin DC, Schoenfield LS, Ramamurthy S. A controlled trial of transcutaneous electrical nerve stimulation (TENS) and exercise for chronic low back pain. N Engl J Med 1990; 322: 1627-34.
- Sachs BL, David JAF, Olimpio D, Scala AD, Lacroix M. Spinal rehabilitation by work tolerance based on objective physical capacity assessment of dysfunction. Spine 1990;p 15: 1325-32.
- Mitchell RI, Carmen GM. Results of a multicenter trial using an intensive active exercise program for the treatment of acute soft tissue and back injuries. Spine 1990; 15: 514-21.
- Donchin M, Woolf O, Kaplan L, Floman Y. Secondary prevention of low back pain. A clinical trial. Spine 1990; 15: 1317-20.
- Manniche C, Lundberg E, Christensen I, Bensen I, Hesselsoe G. Intensive dynamic exercises for chronic low back pain: a clinical trial. Pain 1991; 47: 53-63.
- Manniche C, Hesselsoe G, Bantzen L, Christensen I, Lundberg E. Clinical trial of intensive muscle training for chronic low back pain. Lancet 1988; ii: 1473-6.
- Kellett KM, Kellett DA, Nordholm LA. Effects of an exercise program on sick leave due to back pain. Phys Ther 1991; 71: 283-93.
- Lindstrom I, Ohlund C, Eek C, Wallin L, Peterson L-E, Nachemson A. Mobility, strength and fitness after a graded activity program for patients with subacute low back pain. Spine 1992: 641-52.
- Koes BW, Bouter LM, Beckerman H, van der Heijden GJMG, Knipschild PG. Physiotherapy exercises and back pain: a blinded review. BMJ 1991; 302: 1572-6.
- Goldman L. Changing physician's behaviour [editorial]. N Engl J Med 1990; 322: 1524-5.
Professor Gordon Waddell, DSc, MD, FRCS
Department of Orthopaedic Surgery
Western Infirmary
Glasgow G11 6NT
United Kingdom