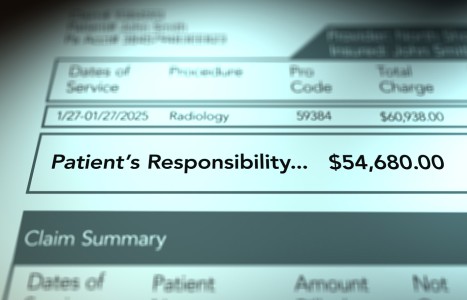
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Understanding Heart Sounds, Part I
With heart disease still America's number one killer, a good assessment of your patient's cardiac status can not be emphasized enough. Other than obtaining a good history, cardiac auscultation will yield the best clue to your patient's status. The key to good auscultation lies in both proper use of the stethoscope and a quiet environment. Stethoscope tubing should be no longer than 12 inches long to prevent distortion of sound. Ear pieces should point towards and fit snuggly into the external ear canal. A stethoscope with both a diaphragm, for listening to high pitched sounds, and a bell, for low pitched sounds, is recommended. The room should be as free of distracting noises as possible.
A good, detailed history should be obtained prior to the exam. Also, be sure to include a family history and diet history. These may provide valid clues to a multitude of predisposing factors to heart disease.
Although inspection, palpation, and according to some sources, percussion precedes auscultation, I will strictly address auscultation in this article. Let us begin with the basic heart sounds. S1 and S2 should be the first identifiable heart sounds. S1 precedes S2 and they can be described simply as the basic "lub-dub" sounds. According to DeGowan and DeGowan,1 the basic heart sounds result from the vibrations of the left ventricular muscle, cardiac skeleton, the valves and great vessels, and the momentum and velocity of the blood as it flows through the elastic system." For our purposes, we will refer to S1 and S2 sounds as the result of closure of the A.V. or mitral and tricuspid valves, and the aortic and pulmonic valves respectively.
With this in mind, let us review the cardiac cycle. We will begin with diastole when blood flows into both the right and left atria through open A.V. valves. At the end of diastole, when the atria contract, increased blood flow into the ventricles causes a rise in the ventricular filling pressure, causing the mitral and tricuspid valves to snap shut, thus producing the S1 or first heart sound.2
During systole the ventricles contract, exerting pressure which eventually rises higher than the pressure of the aorta and the pulmonary artery, forcing the aortic and pulmonic valves open. Eventually at the end of systole the pressure within the ventricles starts to fall as the ventricles start to eject blood. As the pressure drops below the pressure in the aorta, and pulmonary artery, the aortic and pulmonic valves snap shut, eliciting the S2 or second heart sound.3
Now that we have established that the closure of certain valves are manifest as certain heart sounds, let us discuss the phenomena of split heart sounds. When S2 occurs, it is essentially the closure of the louder aortic or A2 valve first followed by the pulmonic or P2 valve closing a split second later. This is referred to as physiologic splitting and normally occurs on inspiration when there is an increased venous return and negative intrathoracic pressure which delays the emptying of the right ventricle and thus delays the closure of the pulmonic valve. It basically sounds like "lub/dubdub." The two sounds should normally be fused on expiration. The S2 sound can best be auscultated with the diaphragm at the second interspaces or intercostal spaces on the right for the aortic closure and on the left for the pulmonic closure.
The S1 sound is also split into a louder mitral sound which precedes a softer tricuspid sound. As you can see, sounds originating from the left side of the heart tend to be louder since the pressure tends to be higher on the left. S1 sound is best heard at the apex of the heart. Since mitral closure is louder and may mask tricuspid closure, you may not be able to hear the S1 split as easily as the S2 split.
In addition to the above basic cardiac sounds, other sounds may be auscultated in correlation to specific events in the cardiac cycle. Although not considered normal, the opening of the aortic valve may be accompanied by a high-pitched "ejection sound" best heard over the aortic auscultatory point. This sound, when heard, follows S1 and may suggest aortic valve stenosis, systemic hypertension, or dilated aorta.4
Another valvular sound, the "opening snap," may be auscultated at the apex as a high-pitched sound. This is the opening snap of the mitral valve. Not normally audible, this sound may clue you into the existence of mitral stenosis. It usually closely follows S2. As the ventricles fill following opening of the A.V. valves, a third heart sound may be auscultated. This sound is due to the rapid filling of the ventricles and is referred to as the S3 sound or ventricular gallop. It follows S2 in the cardiac cycle and may be confused with an S2 split. However, remember that an S2 split should normally split on inspiration whereas an S3 will not. It is a lower pitched sound than the S2 and can best be heard with the bell. S3 sound is considered by most sources to be normal in children and young adults,5 but suggests ventricular dysfunction or left ventricular hypertrophy in adults over 40.6
The S4 sound or atrial gallop precedes S1 and is the result of vigorous atrial contraction. It occurs in patients with hypertension, aortic stenosis, or acute myocardial infarction.7 According to Homma et al.,8 S4 has also been studied in patient's with left ventricular hypertrophy.
The occurrence of both S3 and S4 is a summation gallop and is described as sounding similar to a horse's gallop.
To summarized the auscultatory findings mentioned thus far, the following schematic may be helpful:
S4 | S1 | Ej | S 2 | OS | S3 |
atrial | M/T | aortic v | A2 /P2 | mitral v | ventricular |
contraction | closure | opening | closure | opening | filling |
Further investigation of the S2 split is necessary to complete our study of cardiac auscultation. Remember that S2 sound is made up of the louder aortic sound (A2), which precedes the softer pulmonic sound (P2). The S2 split is, once again, normally auscultated in inspiration and presents as two distinct sounds. This is referred to as a normal or physiologic split. If at any time the split does not present itself in this manner, further investigation is called for. For example, a right bundle branch block (RBBB) may alter the S2 split.
Normally the right and left bundle branches of the cardiac conduction system transmit impulses simultaneously, resulting in depolarization of the lateral walls of the heart at the same time. However if a bundle branch block occurs, depolarization occurs earlier to the unaffected ventricle.9 As a result, valvular, particularly semilunar valve closure, is delayed on the blocked side. Consider what would happen to the S2 split in a patient with a RBBB. Delayed conduction to the right side of the heart would delay closure of the pulmonic valve. As a result the split would be heard regardless of respiratory cycle. It would be heard during expiration and the span between the closure of A2 and P2 would be wider during inspiration. This is referred to as a wide split. Other causes of a wide split would be anything that causes early closure of the aortic valve, such as premature left ventricular contractions, or mitral regurgitation.
Paradoxical or reverse splitting occurs during expiration, but is absent on inspiration, as most commonly seen in a left bundle branch clock, or LBBB. A LBBB delays closure of the aortic valve, which normally closes first. As a result the pulmonic valve closure occurs first, so that your split consists of P2-A2. A LBBB may also cause the S2 split to present as a single sound.10 Other causes of reversed split include premature right ventricular contractions and systemic hypertension.
Fixed splitting does not change with inspiration and can be auscultated in patients with atrial septal defect.11
On conclusion, aside from history, auscultation in the most diagnostic tool when assessing cardiac status. A good history and physical exam should alert you to the development of new cardiac symptomatology or the worsening of a previous cardiac disorder. As primary care physicians we do our patients a disservice by not using our physical assessment skills and in the event that any of the changes just mentioned are discovered, referral to a good cardiologist with a favorable opinion of chiropractic is warranted.
References
- DeGowan, DeGowan. Beside Diagnostic Examination, 5th ed., Macmillan Pub. Co. New York, 1982.
- Yacone-Morton LA. Cardiac assessment. R.N. 54(12) 28-35, Dec. 1991.
- Bates B. A Guide to Physical Examination, 4th ed., J.B. Lippincott Co., Philadelphia, 1987.
- Meyers D. A review of cardiac auscultation, Part I. Hospital Medicine, (29)25-52, Oct. 1993.
- Ibid.
- Folland E, et al. Implications of third heart sounds in patients with valvular heart disease. New England Journal of Medicine, 327(7), 458-62, Aug. 23, 1992.
- Homma S, et al. Relationship of auscultatory fourth heart sounds to the quantitated left artial filling fraction. Clinical Cardiology, 14:671-674, Aug. 1991.
- Ibid.
- Guyton A: Textbook of Medical Physiology, 7th ed., W.B. Sanders Co., Philadelphia, 1986.
- Oravetz J, et al. Dynamic analysis of heart sounds in right and left bundle branch blocks. Circulation, 36:275-283, Aug. 67.
Arlene Tilson-Chrysler, RN, DC
Houston, Texas