Some doctors thrive in a personality-based clinic and have a loyal following no matter what services or equipment they offer, but for most chiropractic offices who are trying to grow and expand, new equipment purchases help us stay relevant and continue to service our client base in the best, most up-to-date manner possible. So, regarding equipment purchasing: should you lease, get a bank loan, or pay cash?
Spinal Stenosis and Dermatomal Evoked Potentials
Spinal stenosis represents a narrowing of the spinal canal, occur either laterally (apophyseal region), or foraminally, both capable of causing root compression, and central/midline (laminar region), causing cord, thecal sac, or cauda equina compression. Spinal stenosis is most commonly central and multilevel in nature, but single level stenosis and lateral recess entrapment may be seen. Spinal stenosis may be congenital, due to conditions like achondroplasia, or acquired/degenerative, due to degeneration of the three-joint-complex and motion segment.
Central Stenosis
Midline compression may be a sequella of degenerative disc disease associated with diffuse annular bulges, spondylosis, buckling of the ligamentum flavum, or overgrowth of the facet joints. Degenerative spondylolisthesis may also contribute to central stenosis. It may also occur subsequent to surgical fusion.
Lateral Stenosis
Nerve roots may get entrapped as they pass under the medial border of the superior articular facet and pedicle to emerge from the IVF. Hypertrophy of the facets due to degenerative change can entrap the nerve in this area know as the "lateral recess" or subarticular gutter. Canal size is an important consideration especially with patients presenting with myelopathy or disc herniation. A small canal in a patient even with a small disc bulge or herniation may produce significant neurological deficits.
Verbiest has classified canal sizes into two types: absolute and relative stenosis. Absolute stenosis represents a spinal canal with an AP diameter of 10 mm or less. Relative stenosis represents a spinal canal of about 10-13 mm in its AP diameter. Studies have demonstrated that small canal size predisposes a patient to neurological injury subsequent to trauma such as an MVA.
Clinically, patients with lumbar stenosis will present with back pain extending into the buttocks, thighs, or legs brought on by prolonged standing or walking. Forward flexion to reduce the lumbar lordosis will often alleviate symptoms. This has been called "the stoop test." Often the patient will experience pain after walking with cessation of pain after they discontinue walking. This has been termed "pseudo-claudication." It is differentiated from vascular claudication and disc extrusion by sitting, which gives a patient relief in spinal stenosis. Walking down a ramp or up a hill will increase the patient's pain. Neurologic deficits are patchy and they may or may not be present during sensory, motor, and reflex examinations. Since the nervous system adapts over time and the development of stenosis is slow and gradual, it takes time for sufficient axonal damage to occur in order and cause symptoms. This is analogous to carpal tunnel syndrome where electrodiagnostic changes often precede overt symptoms. Electrodiagnostic testing is a useful tool to assess patient suspected of having spinal based on neuro-imaging tests such as CT and MRI.

White and Panjabi have suggested using Pavlov's ratio on cervical spine lateral radiographs to determine the existence of a narrow cervical canal. It is believed that a narrow spinal canal of less than 15 mm is an important prognosticator for neurologic deficit and damage in patients with cervical trauma. Pavlov's ratio is determined by the ratio of the anterior to posterior distance of the vertebral body and the distance from the posterior vertebral body to the spinolaminar line. A ratio of one or greater is considered normal, a ratio less than 0.8 mm is suggestive of spinal stenosis. However, CT and/or MRI scans are the imaging techniques of choice to document spinal stenosis. CT gives better delineation of bone changes; MRI has an advantage since it too can document spinal stenosis with its effect on surrounding soft tissue and neural elements.
Electrodiagnostic evaluation typically consists of nerve conduction studies and electromyography which may help identify the level of root entrapment. Another test which offers high sensitivity, specificity, and predictive value is Dermatomal Somatosensory Evoked Potentials (DSEP). In a study by Stolov and Slimp, 25 of 26 (90 percent) patients with spinal stenosis had bilateral abnormal DSEPs, while only 59 percent had EMG abnormality. In another study by Tokuhashi, 90 percent of 34 patients with lumbar spinal stenosis had abnormal DSEPs. In a study by Snowden et al., DSEPs were found to be a useful diagnostic test of CT/MRI documented spinal stenosis. In 54 patients with stenosis, they found a 78 percent sensitivity for those cases with multiple root or multilevel disease, and 93 percent sensitivity single level disease. They defined abnormal DSEP findings as:
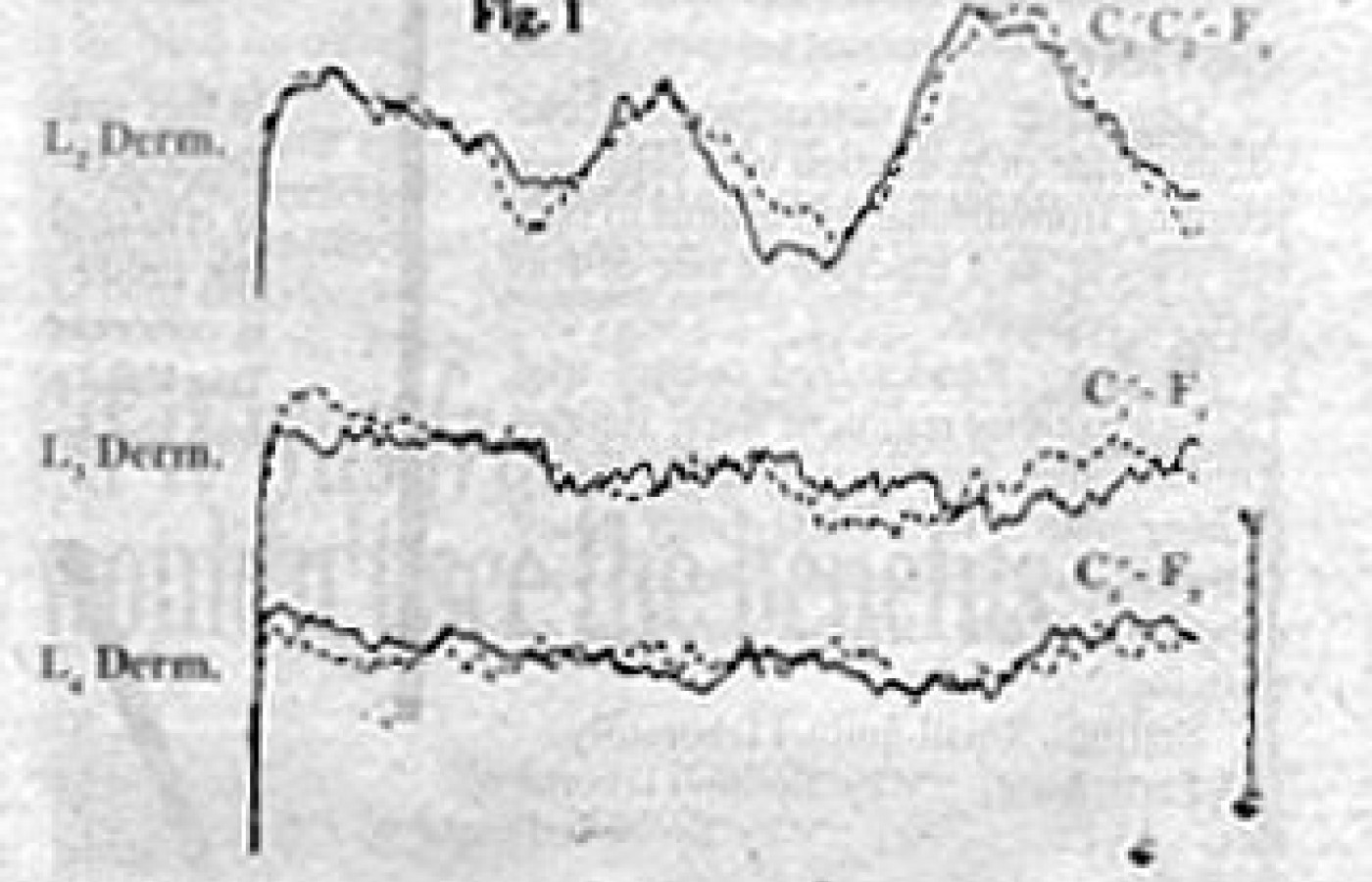
1) absent or prolonged N1 latency greater than 2.5 SD;In a prospective study done by Keim et al., 20 patients with spinal stenosis were found to have a high incidence of posterior tibial nerve (95 percent) abnormality and peroneal nerve abnormalities in 90 percent of the patients with spinal stenosis. They concluded SEPs were a useful electrodiagnostic test for patients with spinal stenosis. Kondo et al., found stress SEPs to be useful in 37 patients with spinal stenosis. Since walking increases pain, they performed SEPs before and after having the patients walk on a treadmill. Thirty-one of 37 patients tested showed significant abnormalities on stress SEP testing. DSEP findings in cases of spinal stenosis will most typically show an absence of normally expected waveforms. Note Figure 1 where dermatomes tested were absent by the lack of discernable peaks or waveforms.
2) side to side latency differences greater than 2.0 SD;
3) amplitude differences greater than 2.0 SD;
4) amplitude ratios greater than 2.0 SD.
DSEPs are a reliable, noninvasive, well tolerated diagnostic test to help delineate the extent of neural compromise in cases of spinal stenosis. Snowden's study found a 93 to 94 percent positive predictive for DSEPs. As always electrodiagnostic studies must be correlated with clinical history, examination findings, and CT/MRI imaging.
References
Croft AC, Foreman SM. Whiplash Injuries, Williams and Wilkins.
Hpp E. Spinal stenosis. Spine, state of the art reviews. 1:3, May 1987 pg. 367.
Keim et al. Spine 10:4, 1985, 338-350.
Kondo M, Matsuda H. Electrophysiological studies of claudication in spinal stenosis. Spine 1990, pg. 862.
Snowden et al. DSEP in the diagnosis of lumbosacral spinal stenosis. Muscle and Nerve, Sept. 92, pg. 1036.
Stolov WC, Slimp JC. DSEP in lumbar spinal stenosis. Paper presented at the 1988 American Assoc. of EMG and Electrodiagnosis.
Swenson RS. JNMS Vol. 2, No. 2, 1994.
White A, Panjabi M. Clinical Biomechanics of the Spine. JB Lippincott.
David BenEliyahu, DC, DABCT, DABCSP
Selden, New York