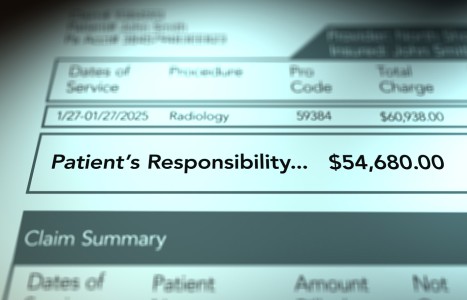
Recent laws in New Jersey and California represent a disturbing trend that will negatively impact a practice’s ability to collect monies from patients, as well as expose them to significant penalties if the practice does not follow the mandatory guidelines to a T. Please be aware that a similar law may be coming to your state. The time to act is before the law is passed.
Morning Stiffness
Does morning stiffness refer to actual stiffness/tightness or pain or a combination of the two? Clearly patients are complaining of difficulty in movement. Some patients take a warm shower and stretch and are symptom free to the next morning; for others the stiffness and pain persists for hours and then recedes with increased movement, only to return later in the evening.
As Gifford1 states, morning stiffness is linked to "changes in range of movement, fluid accumulation, weakness and perceptual and reflexogenic factors associated with nociceptive and central pain mechanisms." An inflammatory arthropathy is often blamed for morning stiffness and the decrease in this stiffness is often used as a measure of the effectiveness of treatment.2
In the morning there is normally less lumbar flexion than later in the day.3 This is probably due to fluid accumulation of the disc during the night. First thing in the morning the spine will be more mechanically stiff due to the swollen discs. The avascular disc requires continuous pressure changes for its survival. Not only does gravity affect the fluid interchange but discs are also affected by muscular forces and viscoelastic deformation of the annular fibers. Gossman4 showed that immobilization of muscle can result in shortening within a few hours. In the shortened position the amount of sarcomeres decreases. Viscoelastic tissues elongate with load and slowly shorten when the load is decreased or eliminated. Gifford1 feels that due to the perception of stiffness the central nervous system might increase resting muscle tone and inhibit movement to protect the musculoskeletal tissues after prolonged inactivity.
Morning stiffness may also be related to glycosaminoglycan hyaluronic acid (HA) which is in the extracellular portion of all connective tissues including discs. HA attracts water and also resists water flow.5 Connective tissue accumulation of HA causes increased rigidity of tissue and restricts joint and muscle motion. Activity forces HA out of the tissues into the lymphatics and plasma. In the early morning the plasma levels are low, indicating an increase in the interstitial tissue concentrations and resulting in stiffness. Plasma levels of HA double after being up and active for one hour.6 Increased output of HA is stimulated during inflammation by the kinin, interleukin-1, and HA levels increase when inflamed tissues are at rest.1
Bogduk and Twomey7 found that disc injury causes increased disc pressure, which can cause pain by stretching the innervated peripheral annulus. This may explain why an acute disc patient is worse in the morning, when changing from the lying to sitting position. Gifford1 states that these patients will benefit in the morning by doing several minutes of gentle lumbar movements before rising. This movement may expel some fluid (including inflammatory exudate) from the disc, reducing discal pressure. The reduction in discal pressure may also cause the CNS to reduce its inhibitory effect, causing increased muscle tone.
Did you ever notice that a patient may feel good while receiving traction and feel pain when the traction is released or upon getting up from the traction table? This is an example of increasing discal pressure (as during a nights sleep) and the result of immediate motion. Again, immediately after the traction, a pelvic rock and rotational exercise might help. The presence of pain in this scenario may also be an indication of a hydrostatically intact disc since normal fluid dependent behavior occurred.8
Gifford1 gives an interesting history of a patient with chronic morning stiffness for two hours, which freed up during the day with movement. The stiffness continued until the patient developed posterior thigh pain, which continued for 8 to 10 weeks. After the thigh pain left the patient was rid of his morning stiffness. Is it possible that the morning stiffness was due to an inflammatory disc mechanism affecting the fluid exchange as explained above? Could it be that the patient developed a radial fissure in the annulus resulting in a loss of the fluid mechanism, and therefore the loss of stiffness?
References
- Gifford L. Fluid movement may partially account for the behaviour of symptoms associated with nociception in disc injury and disease. Shacklock MO. Moving in on Pain. Australia, Butterworth-Heinemann, 1995.
- McKenna F, Wright V. Pain and stiffness in the rheumatic diseases: The relevance of a diurnal variation to diagnosis. British Journal of Rheumatology 29 (Suppl 1):24, 1990.
- Wing P, Tsang I, Gagnon F, et al. Diiurnal changes in the profile shape and range of motion of the back. Spine 17 (7): 761-766, 1992.
- Gossman M, Sahrmann S, Rose S. Review of length associated changes in muscle. Physical Therapy 62:1799-1808, 1982.
- Laurent T. Biochemistry of hyaluronan. Acta Otolaryngology (Suppl)442:7-24,1987.
- Lindqvist U, Engstrom-Laurent A, Laurent U et al. The diurnal variation of serum hyaluronan in health and disease. Scandinavian Journal of Clinical and Laboratory Investigation 48 (8):765-770, 1988.
- Bogduk N, M Twomey L. Clinical Anatomy of the Lumbar Spine. Melbourne, Churchill Livingstone.
- Porter R, Trailescu I.Diurnal changes in straight leg raising. Spine 15 (2):103-106, 1990.
Warren Hammer, MS, DC, DABCO
Norwalk, Connecticut